[1]
Deng J, Zhang H, Wang YP, Liu Q, Du M, Yan WX, et al. Global, regional, and national burden of dengue infection in children and adolescents: an analysis of the Global Burden of…
Introduction: Effective detection methods to distinguish between transient human papillomavirus (HPV) infection and clinically relevant high-risk HPV (hrHPV)-induced diseases are lacking, leading to excessive referrals and overtreatment. This study evaluated the clinical performance of a host DNA six-methylation marker panel (ASTN1, DLX1, ITGA4, RXFP3, SOX17, and ZNF671) to triage Chinese women who were hrHPV-positive.
Methods: This prospective multicenter study enrolled women aged 21–65 years with positive hrHPV testing. hrHPV genotyping, cytology, colposcopy, and the six-methylation marker assay were performed. High-grade cervical lesions were defined as histologically confirmed CIN2+. Forest plots analyses were performed to assess the triage performance of the methylation assay.
Results: Of the 1,806 patients recruited from 4 hospitals in China, 1,659 were included. The methylation assay positivity rates were 7.5%, 73.9%, 88.9%, and 100% for CIN1, CIN2, CIN3, and cervical cancer, respectively. The six-methylation marker assay demonstrated sensitivities of 82.2% and 90.3% and specificities of 92.4% and 84.1% for CIN2+ and CIN3+, respectively, which were higher than those of HPV genotype testing and cytology (≥ASCUS) screening; the areas under the curve for CIN3+ detection were 0.87 (0.84–0.90), 0.68 (0.64–0.72), and 0.64 (0.60–0.69), respectively. The six-methylation marker assay showed the lowest colposcopy referral rate (24.2%) and required the fewest referrals for detection, with 1.32 and 2.39 referrals per CIN2+ and CIN3+ cases, respectively. In women aged <30 years, the six-methylation marker assay had the highest specificity for CIN2+ (95.7%) and a sensitivity and specificity for CIN3+ of 80.8% and 88.9%, respectively. It had the lowest referral rate (17.17%) and colposcopy referrals, with 1.24 and 2.43 per CIN2+ and CIN3+ cases, respectively.
Conclusions: The host DNA six-methylation marker assay is a reliable triage tool for women who are hrHPV-positive, providing evidence supporting the application of methylation markers in China.
Cervical cancer is the second most common gynecological malignancy that causes death among female patients, with approximately 529,800 new cases and 275,100 deaths annually worldwide. Notably, China accounts for 28% of global cases and 50% of new cases in Asia each year, representing 25%–33% of the annual deaths in Asia (1). Persistent infection with hrHPV is considered the primary cause of cervical cancer and its precancerous lesions. However, HPV genotype testing demonstrates a low specificity of only 31.8% for CIN3 and worse (2). This is because most HPV infections are transient and clear naturally, especially in women younger than 30 years, who have regression rates of 60% (3). Therefore, given China’s large population and the substantial number of women who test HPV-positive annually, a reliable triage tool for high-grade intraepithelial lesions (HSIL) is urgently needed.
Ideal triage strategies require a balance between safety, sensitivity, specificity, and screening-related burden; however, a consensus on the optimal triage test is lacking. Various triage methods have been proposed, including p16/Ki-67 cytological dual staining and methylation assays. While p16/Ki-67 staining demonstrates 90% sensitivity for CIN3+, its limited specificity (42%) fails to reduce colposcopy referral rates (4). A meta-analysis showed that the sensitivity and specificity of all methylation assays for CIN3+ were 0.708 and 0.780, respectively (5). Among these, a methylation panel comprising six markers (ASTN1, DLX1, ITGA4, RXFP3, SOX17, and ZNF671) is suitable for application in developing countries due to its superior specificity (88.7%–94.6%) for CIN3+ (3,6). However, data for this methylation panel come only from clinical trials conducted in Western countries, and the prevalence and distribution of HPV genotypes in China differ from those in Western countries, with significantly higher infection rates of HPV52 and HPV58. Furthermore, the applicability of the positive threshold of this methylation panel to Chinese women and differences in the expression of methylation markers are unclear.
Therefore, this study hypothesized that the methylation pattern in China might be distinct and conducted a prospective multicenter study to evaluate the clinical performance of a host DNA six-methylation marker panel in Chinese women who were hrHPV-positive. This was the first prospective multicenter study in China with a large sample size to evaluate the feasibility of the six-methylation marker assay as a triage tool for hrHPV-positive women.
Overall, 1,806 women from the colposcopy clinics of 4 hospitals across China underwent HPV genotype testing, cytological screening, methylation assays, and colposcopy between August 2018 and April 2021. The participating institutions included Peking University First Hospital, Nanjing Drum Tower Hospital, Hunan Provincial Maternal and Child Health Care Hospital, and The First Affiliated Hospital of Anhui Medical University, representing 4 different provinces. The inclusion criteria were as follows: 1) women aged 21–65 years with an intact cervix, 2) hrHPV-positive status with available cervical cytology results, and 3) cervical lesions confirmed through colposcopy biopsy. The exclusion criteria were as follows: 1) pregnant, maternal, or lactating women; 2) unwillingness to participate or inability to provide informed consent; and 3) a history of cervical cancer. This study received ethical approval from all 4 participating hospitals (ethics approval numbers: JNFL2020001, 2020-180-04, JNFL2018001, and PJ 2021-02-06).
Samples were obtained by experienced gynecologists using a cervical brush. Cytology screening employed the liquid-based cytology (LBC) method, and the diagnosis was classified into 5 levels according to the 2014 Bethesda System (TBS) criteria. HPV genotype testing was performed using fluorescence quantification PCR, and results were categorized into 2 groups: HPV16/18-positive and positive for the other 12 hrHPV genotypes, i.e., “other-hrHPV positive.” Host DNA from LBC samples was heavy sulfite-transformed for methylation analyses. The methylation panel comprised 6 gene markers: DLX1, ASTN1, ITGA4, RXFP3, SOX17, and ZNF671. All procedures were performed according to standardized instructions. ZNF671 was assigned a score of 3 points, while the other 5 methylation markers were assigned 1 point each. The six-methylation marker assay was considered positive if the cumulative score across all 6 markers was ≥3. All HPV genotyping and methylation assays were conducted in a central laboratory. All women underwent colposcopy, and cervical biopsies were performed based on colposcopic impressions. Cervical lesions were histologically classified as CIN1/2/3 or cervical cancer (CC), while those with normal biopsy results or colposcopic impressions were categorized as “normal.”
This study evaluated 5 triage strategies for detecting CIN2+ and CIN3+ in hrHPV-positive women using histopathology as the gold standard. The evaluated strategies were as follows: 1) HPV16/18 genotyping; 2) cytology (≥ASCUS); 3) six-methylation marker assay; 4) six-methylation marker assay and HPV16/18 co-screening; and 5) six-methylation marker assay and cytology (≥ASCUS) co-screening. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), area under the receiver operating characteristic curve (AUC), and forest plots were calculated for each method. Statistical analyses were performed using SPSS (version 26.0, IBM Corp., NY, USA) and R (version 4.1.2, R Core Team, Vienna, Austria). Independent-sample t-tests were used to compare normally distributed continuous data, whereas nonparametric continuous variables were analyzed using the Mann-Whitney test. Categorical variables were assessed using the chi-squared or Fisher’s exact test. To compare methylation marker scores among different CIN groups that followed a non-normal distribution, this study employed the Kruskal-Wallis test, followed by Dunn’s test for pairwise comparisons. Two-sided P<0.05 were considered significant.
Finally, 144 cases did not meet the inclusion criteria, and 3 cases were excluded due to unsuccessful methylation detection, resulting in 1,659 cases available for final analysis, as shown in Figure 1. Assessment using a mixed-effects model showed no significant center effect (P>0.05) on baseline characteristics or CIN2+/CIN3+ detection rates. Data from all centers were therefore pooled for final analysis. The study flowchart is presented in Figure 1.
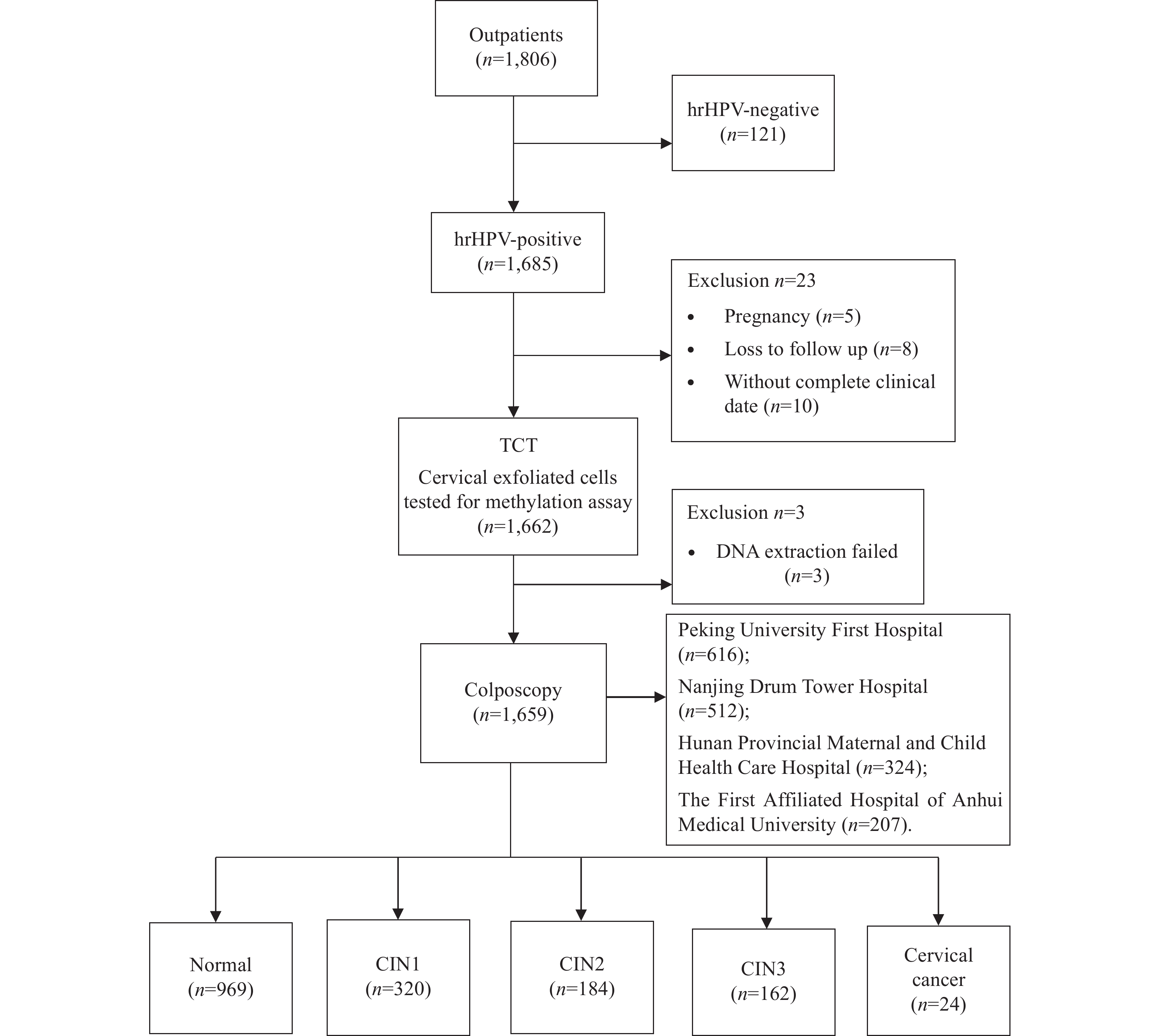
Study flowchart of women who were hrHPV-positive.
Abbreviation: HPV=human papillomavirus; TCT=ThinPrep Cytologic Test; CIN=cervical intraepithelial neoplasia.
The mean patient age was 41.3 years (range: 21–65). Histopathological findings included 320 (19.3%), 184 (11.1%), 162 (9.8%), and 24 (1.4%) cases of CIN1, CIN2, CIN3, and CC, respectively. Among all cases, 37.1% (259/690) were HPV16/18-positive. The methylation assay demonstrated positivity rates of 7.5% (24/320), 73.9% (136/184), 88.9% (144/162), and 100% (24/24) for CIN1, CIN2, CIN3, and CC, respectively. The methylation scores increased significantly with the severity of cervical lesions (P<0.05). Characteristics of the CC screening and methylation assays are presented in Table 1.
Table 1.
Cervical screening and six-methylation marker assay for cervical precancerous lesions and cervical cancer.
The 3 most frequently positive methylation markers in the CIN2+ and CIN3+ groups were ZNF671 (65.8% vs. 88.2%), DLX1 (43.5% vs. 68.3%), and ASTN1 (37% vs. 61.3%). In the CIN1 group, DLX1 showed the highest positivity rate (21.6%). However, as the cervical lesions progressed in severity from CIN1 to CIN2, the positive methylation rate of ZNF671 increased dramatically by 59.2%, which was substantially higher than that of the other markers (
The six-methylation marker assay as a single triage tool demonstrated a sensitivity of 82.2% for CIN2+ and a specificity of 92.4%. This sensitivity was significantly higher than that of HPV16/18 genotyping but comparable to that of cytology (≥ASCUS), while its specificity was the highest among all 3 methods. For CIN3+, the six-methylation marker assay achieved a sensitivity of 90.3% and a specificity of 84.1% (Table 2).
Table 2.
Performance of different triage tools for the detection of CIN2+/CIN3+ among women who were hrHPV-positive.
The AUCs of HPV16/18 genotyping, cytology (≥ASCUS), and the six-methylation marker assay for CIN2+ and CIN3+ were 0.61 and 0.64, 0.69 and 0.68, and 0.87 and 0.87, respectively. Combining the six-methylation marker assay with HPV16/18 genotyping (≥ one positive) as a triage tool for CIN2+/3+ resulted in a higher sensitivity but a lower specificity compared to HPV16/18 genotyping alone. The relative sensitivity and specificity with HPV16/18 genotyping and cytology (≥ASCUS) as the reference strategy for CIN2+ and CIN3+ are shown in Figures 2 and 3.
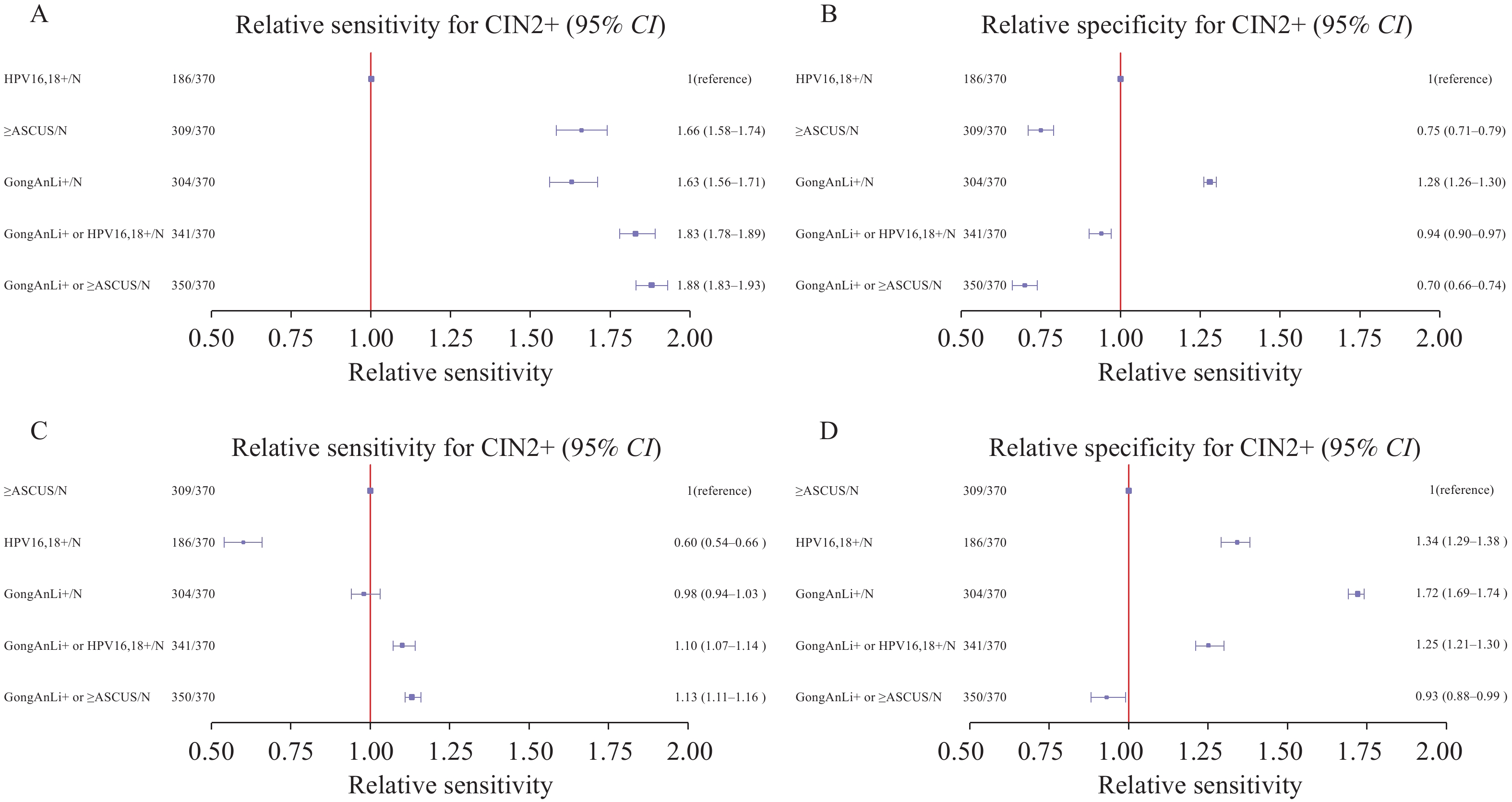
Forest plots showing the relative sensitivity and specificity for CIN2+ detection of different triage tools compared with HPV16/18 genotyping and cytology (≥ASCUS). The relative (A) sensitivity and (B) specificity of different triage tools compared with HPV16/18 genotyping; The relative (C) sensitivity and (D) specificity of different triage tools compared with cytology (≥ASCUS).
Abbreviation: CIN2+=cervical intraepithelial neoplasia grade 2 or worse; HPV=human papillomavirus; ASCUS=atypical squamous cells of undetermined significance.
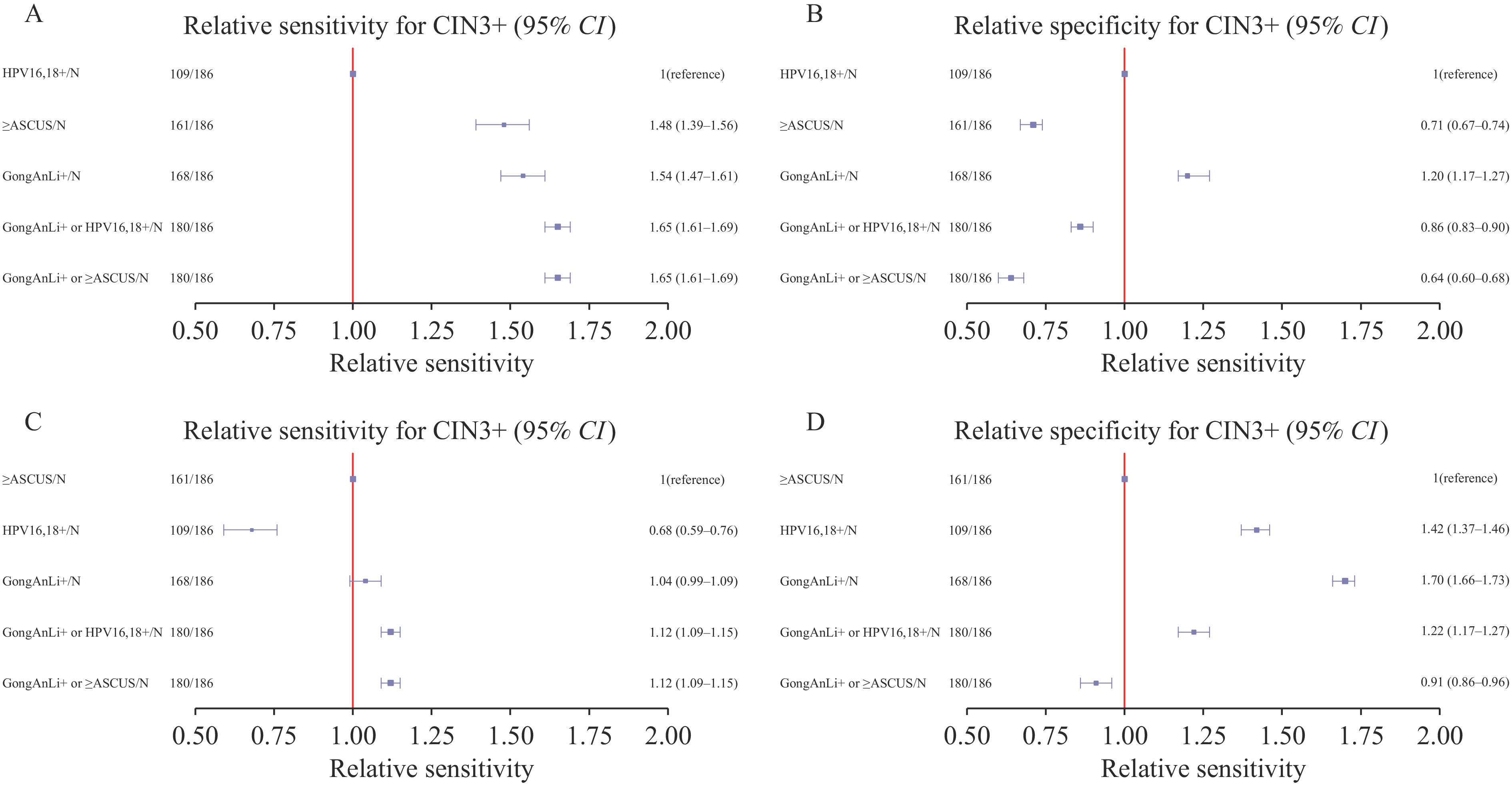
Forest plots showing the relative sensitivity and specificity for CIN3+ detection of different triage tools compared with HPV 16/18 genotyping and cytology (≥ASCUS). (A) The relative sensitivity of different triage tools compared with HPV 16/18 genotyping; (B) The relative specificity of different triage tools compared with HPV 16/18 genotyping; (C) The relative sensitivity of different triage tools compared with cytology (≥ASCUS); (D) The relative specificity of different triage tools compared with cytology (≥ASCUS).
Abbreviation: CIN2+=cervical intraepithelial neoplasia grade 2 or worse; HPV=human papillomavirus; ASCUS=atypical squamous cells of undetermined significance.
This study further analyzed the efficacy of different triage tools in women aged <30 years. The DNA methylation positivity rate among women who were <30 years of age and hrHPV-positive was 17.2% (51/297), which was lower than that among women >30 years of age (25.8%). The combination of the six-methylation marker assay and cytology had the highest sensitivity for CIN2+ (89.2%). However, the six-methylation marker assay showed the highest specificity (95.7%), with relative specificities of 1.34 and 1.8 compared to HPV genotyping and cytology (≥ASCUS), respectively. For CIN3+ detection, the six-methylation marker assay demonstrated relatively good sensitivity and specificity, with values of 80.8% and 88.9%, respectively (
In addition, the six-methylation marker assay demonstrated the lowest colposcopy referral rate (24.23%) and the fewest referrals required for detection, with 1.32 and 2.39 referrals per CIN2+ and CIN3+ cases, respectively. In contrast, HPV16/18 genotyping and cytology (≥ASCUS) required approximately 3 referrals each per CIN2+ case, and 5.02 and 5.61 referrals per CIN3+ case, respectively. In the subgroup analysis of women <30 years of age, the six-methylation marker assay also demonstrated the lowest colposcopy referral rates (17.17%) and colposcopy referrals (

As we age, chronic low-level inflammation, often called “inflammaging”, can quietly affect our health, increasing the risk of heart disease, diabetes, and cognitive decline. Recent research highlights cocoa extract as a natural ally against…

– Advertisement –
– Advertisement –
– Advertisement –
BEIJING, Oct. 24 (Xinhua/APP): “Radiance: Ancient Gold Ornaments from the Collection of the Hong Kong Palace Museum” opened at the Capital Museum Wednesday.
The exhibition showcases over…

The company behind the Airlander 10 giant hybrid aircraft has secured its first reservations for use in the military.
Bedford-based Hybrid Air Vehicles (HAV) said three had been reserved by an “innovative defence contractor” looking to make use of Airlander’s unique capabilities.
Airlander 10, which has not yet gone into production, was expected to initially be certified for civil use, but HAV said its versatile nature meant it could be modified to meet the needs of the military market.
George Land, executive director of sales at HAV, said they were “pleased to be working with an undisclosed customer to provide three aircraft for further customisation”.
The Airlander is a combination of an airship and a plane and currently uses four combustion engines and gases to take-off and in flight.
HAV said the Airlander could:
The company said new threats across the globe required new solutions, and Airlander would directly respond to current and emerging threats.
Work on a production facility started last December in Doncaster where it was expected airships would be built and tested in 2026.
The company had previously said the European-based Air Nostrum Group had reserved 10 Airlanders, but that number had increased to 20, for delivery by 2027.
The Airlander has been designed to be about 320ft (98m) long, with a cabin underneath, making it the world’s longest aircraft.
Mr Land said: “Its versatility, high payload, and endurance have always given Airlander 10 obvious advantages over other aircraft in Command, Control, Communications, Computers, Intelligence, Surveillance, and Reconnaissance (C4ISR).
“As warfare evolves to meet current threats this capability is ever more valuable, and we have worked hard to showcase the aircraft’s capabilities.”
He added that they expected other military reservations to follow.
This request seems a bit unusual, so we need to confirm that you’re human. Please press and hold the button until it turns completely green. Thank you for your cooperation!

In a welcome development for Pakistan’s cricket fraternity, the Pakistan Cricket Board (PCB) has reportedly granted No Objection Certificates (NOCs) to several national players for participation in the upcoming 15th edition of the Big…