What are the challenges?
Taking inspiration from Silverstone, Suzuka, and Hockenheim, it’s no surprise that COTA is as popular as it is challenging.
But while many of the corners will feel familiar, its most famous turn is 100% original….

Taking inspiration from Silverstone, Suzuka, and Hockenheim, it’s no surprise that COTA is as popular as it is challenging.
But while many of the corners will feel familiar, its most famous turn is 100% original….
This request seems a bit unusual, so we need to confirm that you’re human. Please press and hold the button until it turns completely green. Thank you for your cooperation!
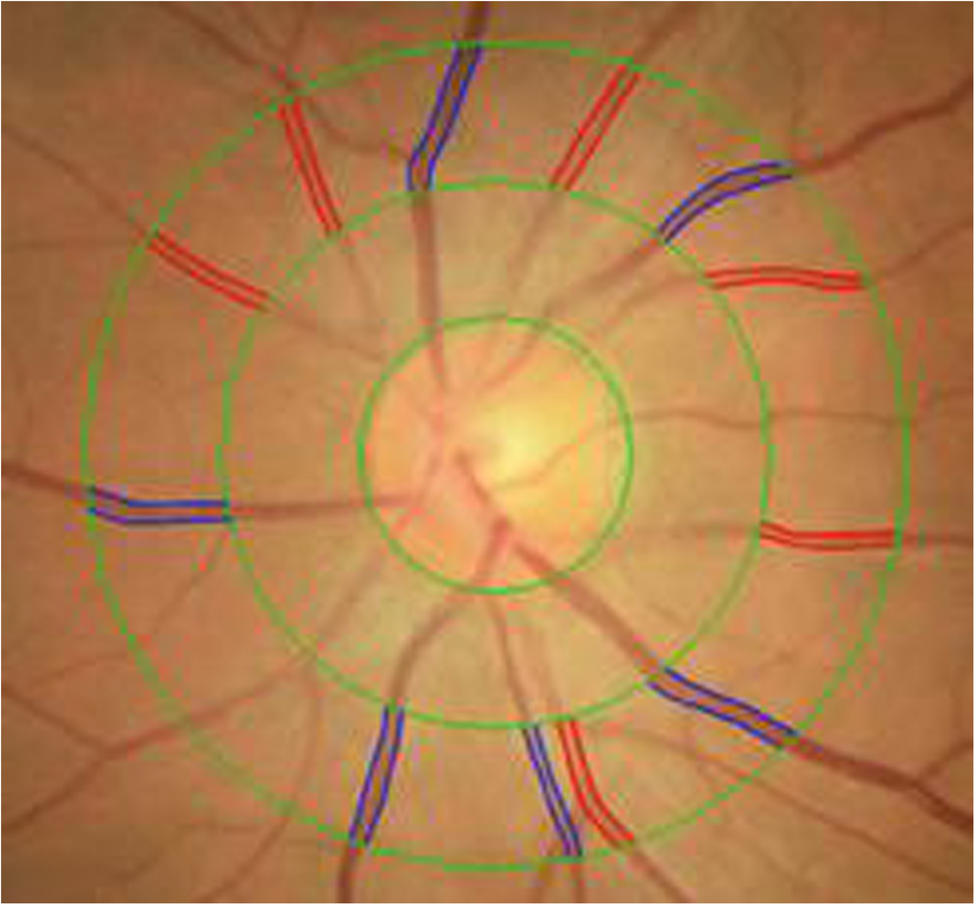
Carmeliet P. Angiogenesis in health and disease. Nat Med. 2003;9(6):653–60.
Google Scholar
Hoon M, Okawa H, Della Santina L, Wong RO. Functional architecture of the retina: development…

It’s safe to say the Nintendo Switch 2 is the game console to get this year, and if you already got your hands on one, you’ve probably loaded it up with all your old Switch games and new Switch 2 games. If you haven’t thought about adding more…

Therabody just revealed a bunch of new products, including the TheraFace Mask Glo. This MF Doom-looking full-face mask offers quite a different experience from the pre-existing TheraFace Pro. The Pro is essentially a face massager, but the Mask…

Andrew Garfield and Sesame Workshop, Katie Couric and the Colorectal Cancer Alliance, the Clinton Global Initiative, Google, Headspace, IFC, MTV Entertainment Studios, Paramount Pictures, Spotify and The Daily Show are among the finalists for…
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll…

Terms
While we only use edited and approved content for Azthena
answers, it may on occasions provide incorrect responses.
Please confirm any data provided with the related suppliers or
…
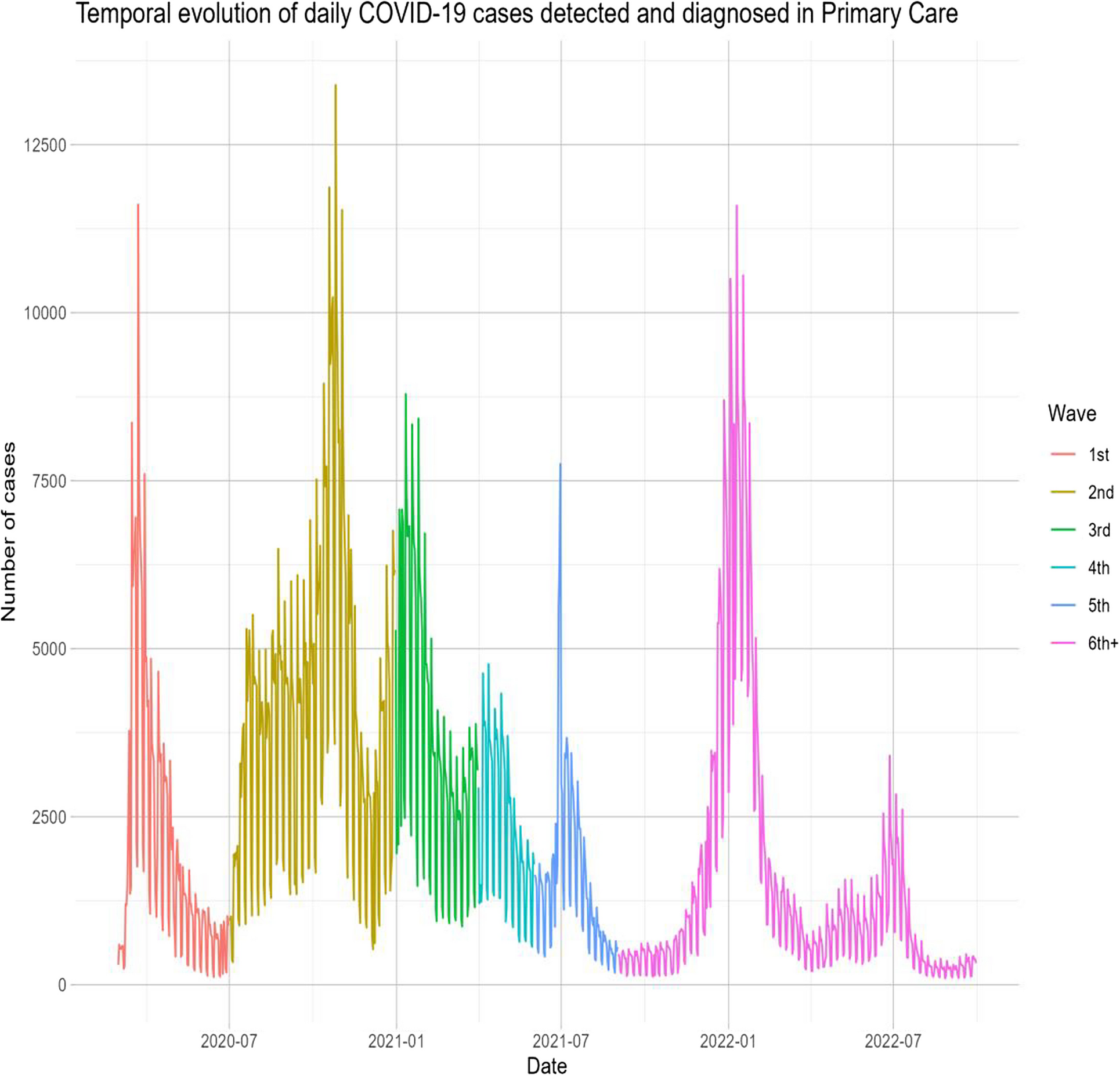
This retrospective study analyzed over 2 million COVID-19 cases from March 2020 to September 2022 across multiple COVID-19 waves, with follow-up 90 days post-diagnosis or until death. Our study underscores the significant impact of COVID-19 on PHC in the initial years of this pandemic in Catalonia. Furthermore, using machine learning models (GLMs, Lasso, Gradient Boosting, SVMs), we identified key predictors of poor outcomes, such as age, social deprivation (MEDEA), blood pressure, and a history of either diabetes, COPD, cardiovascular disease, or obesity. The models showed strong predictive accuracy (AUC: 0.73, 95%CI (0.72;0.73)–0.95, 95%CI (0.94;0.95)). Finally, using these models, an interactive web app was developed for personalized risk estimation (https://dapcat.shinyapps.io/CovidScore).
We found that the CFR was highest during the first wave of the pandemic, gradually decreasing in subsequent waves, with the second wave showing the highest incidence of cases. The higher comorbidity burden observed in the first wave may reflect limited testing availability during that period, which likely focused on more severe cases. The decrease in the CFR may be attributed to a combination of increased immunity (due to vaccination and SARS-CoV-2 infections), better identification of more severe cases, and the lower pathogenicity of recent variants like Omicron. Overall, these findings suggest changes in the SARS-CoV-2 virus, an adaptive response in healthcare, and improvements in the prevention (i.e., via vaccination) and treatment of complications as the pandemic progressed [21].
Regarding predictors of poor prognosis at the time of COVID-19 diagnosis in PHC, we identified older age, epidemic wave, social deprivation, and a history of diabetes, obesity, chronic obstructive pulmonary disease (COPD), cardiovascular disease, hypertension, and dyslipidemia. While study results vary across different populations, numerous studies have identified advanced age and comorbidities such as hypertension, cardiovascular disease, COPD, and diabetes as predictors of increased COVID-19 severity [22,23,24]. Additionally, social deprivation indicators, such as the MEDEA index, have been associated with poorer outcomes in terms of severity and mortality, underscoring the multifactorial nature of COVID-19 outcomes. Understanding and addressing these predictive factors is crucial for improving management and outcomes in affected patients. The inclusion of’epidemic wave’reflects the changing contextual factors, such as virus variants, public health measures, and healthcare strain that significantly influenced outcomes [25]. However, this limits the direct application in future waves. In such cases, the most recent wave may be used as an initial reference, while outcome data are monitored to reassess and recalibrate the model accordingly. Ideally, prediction models should be dynamically updated to remain accurate and clinically useful during future epidemic scenarios.
Conditions associated with low-grade chronic inflammation, such as obesity and diabetes mellitus, are also relevant at the metabolic level [26]. Several systematic reviews have provided consistent evidence that diabetes and obesity are associated with poorer COVID-19 outcomes, which agrees with our study [27]. Although the reasons for this association are not entirely clear, these conditions could exacerbate respiratory problems and/or affect immune responses. A systematic review and meta-analyses on high-risk phenotypes in people with diabetes determined that individuals with a more severe course of diabetes and pre-existing comorbidities had a poorer prognosis of COVID-19 than individuals with a milder course of the disease, highlighting the need for individualized and proactive management strategies for high-risk patients [28].
At the hospital level, predictive models like the ISARIC 4 C have been developed to anticipate clinical deterioration (including mortality, ICU admission, or intubation), assessing age, gender, comorbidities, and nosocomial infection [29]. A similar study in the United Kingdom, utilizing computerized PHC medical records, developed predictive algorithms for COVID-19 mortality and hospital admission risk. Factors such as age, body weight, ethnicity, and social risk explained 73% of COVID-19 deaths and 58% of hospital admissions, suggesting periodic recalibration of these models to reflect the evolving nature of the pandemic [30]. An early pandemic study on PHC identified key risk factors for ICU admission and mortality, including advanced age, male gender, autoimmune disease, bilateral pulmonary infiltrates, and elevated LDH, D-dimer, and C-reactive protein. Protective factors included myalgias, arthralgias, and anosmia [31].
Recent advances in AI and machine learning have significantly contributed to managing the COVID-19 pandemic by aiding in detection, treatment, mortality prediction, and infection modeling to reduce virus spread [32,33,34].
In this study, we used machine learning to develop predictive models and then used these models to develop an app. The app provides comprehensive information to estimate the risk of COVID-19 prognosis outcomes for individuals based on their risk factors (e.g., age, sex, comorbidities, vaccination status, COVID-19 wave). This approach could be used in PHC to identify individuals needing closer monitoring and interventions to prevent serious complications and hospitalization. Moreover, model calibration was assessed using the Brier Score, which integrates both discrimination and calibration aspects. All models showed low Brier Scores, suggesting a high level of agreement between predicted and observed risks. Given the large, representative nature of the dataset, we expect limited calibration drift within this population. Nonetheless, we acknowledge that external validation with calibration plots and slope/intercept assessment would be useful to confirm generalizability in other settings. Although COVID-19 is now endemic, this study highlights the importance of early risk stratification in primary care based on routine data at diagnosis. These findings may inform preparedness for future COVID-19 waves or other infectious outbreaks, where identifying predictors of poor outcomes at diagnosis remains key to guiding timely care.
Our study has limitations inherent to its retrospective design. Outcomes depend on the quality of existing clinical records not specifically collected for this research and have yet to undergo individual validation. Some outcomes may have been underreported or misclassified, especially if they were managed outside the hospital setting or not fully captured in the electronic health records. However, major outcomes such as mortality, hospitalization, and ICU admission are reliably recorded within the system. A notable limitation is the potential impact of vaccine implementation on epidemiology and prognosis, which underscores the need to recalibrate predictive models with post-vaccination data to maintain accuracy. Periodic updates with the latest available data are essential to ensure the continued relevance of these models. Although no predictive model is perfect for COVID-19 patients, our models serve as valuable tools to estimate the risk of complications, helping to identify patients who require closer monitoring. However, the accuracy of these models can be affected by variations in the detection and recording of symptoms and risk factors by different healthcare professionals. Moreover, mild COVID-19 cases may have gone unrecorded in PHC, potentially leading to their exclusion from our study population. Another limitation of our study is that the model was developed using subjects with confirmed COVID-19, whereas in primary care, clinicians often assess patients with suspected infection before test confirmation. This may limit applicability in early diagnostic uncertainty. Moreover, the model remains useful for risk stratification once a diagnosis is confirmed in the primary care setting. Additionally, the study benefits from using the SIDIAP database, which includes a substantial patient cohort and is a well-validated source for epidemiological and pharmaco-epidemiological studies within the Catalan primary care setting. This database not only provides standardized clinical data (including health issues, physical exams, lab results, and medication records) from pseudo-anonymized electronic health records but was also specifically updated to include COVID-19-related variables (such as diagnostic tests and procedures), enabling researchers to conduct targeted epidemiological studies. Despite the fact that we used a large, representative dataset and validated the models on a separate 25% test set, external validation was not performed. This may lead to overestimation of performance. External validation using more recent data or in other populations, such as from different regions, healthcare systems, or countries is needed to confirm the model’s generalizability and ensure robust performance of the predictive models across evolving clinical contexts.

ALISON BEARD: I’m Alison Beard.
ADI IGNATIUS: I’m Adi Ignatius. This is HBR IdeaCast.
ALISON BEARD: Adi, you are very familiar with both of the guests on today’s show. One is a comedian and talk show host, Jimmy…