Patients treated with izalontamab brengitecan (iza-bren; BL-B01D1) had superior overall response rate (ORR) compared with chemotherapy in patients with recurrent or metastatic nasopharyngeal carcinoma (NPC), according to results from the BL-B01D1-301 study (NCT06118333) presented at the 2025 European Society for Medical Oncology (ESMO) Congress and published in The Lancet.1,2
The ORR by blinded independent central review was 54.6% (95% CI, 45.2%–63.8%) with iza-bren vs 27.0% (95% CI, 19.1%–36.0%) with chemotherapy, with an odds ratio of 3.3 (95% CI, 1.9–5.8; P < .0001) showing it was significantly higher in this primary end point.1
“This was the first randomized phase 3 study evaluating iza-bren in recurrent or metastatic NPC. Our study has met its primary end point for ORR, and we can see a clinically meaningful improvement in progression-free survival [PFS] and it has a management safety profile,” said Huaqiang Zhou, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China, in his presentation.1
Approximately 20% to 30% of patients with NPC have recurrent or distant metastases, and current treatment options have low response rates. Iza-bren is a potentially first-in-class topoisomerase 1 inhibitor-based EGFR and HER3 bispecific antibody-drug conjugate (ADC).
The multicenter, randomized, open-label, phase 3 BL-B01D1-301 trial was designed to investigate this agent in patients who had previously received at least 2 lines of systemic chemotherapy including at least 1 platinum-containing regimen and a PD-1 or PD-L1 inhibitor. The primary end points were ORR and overall survival (OS), with secondary end points including progression-free survival, duration of response (DOR), and safety.
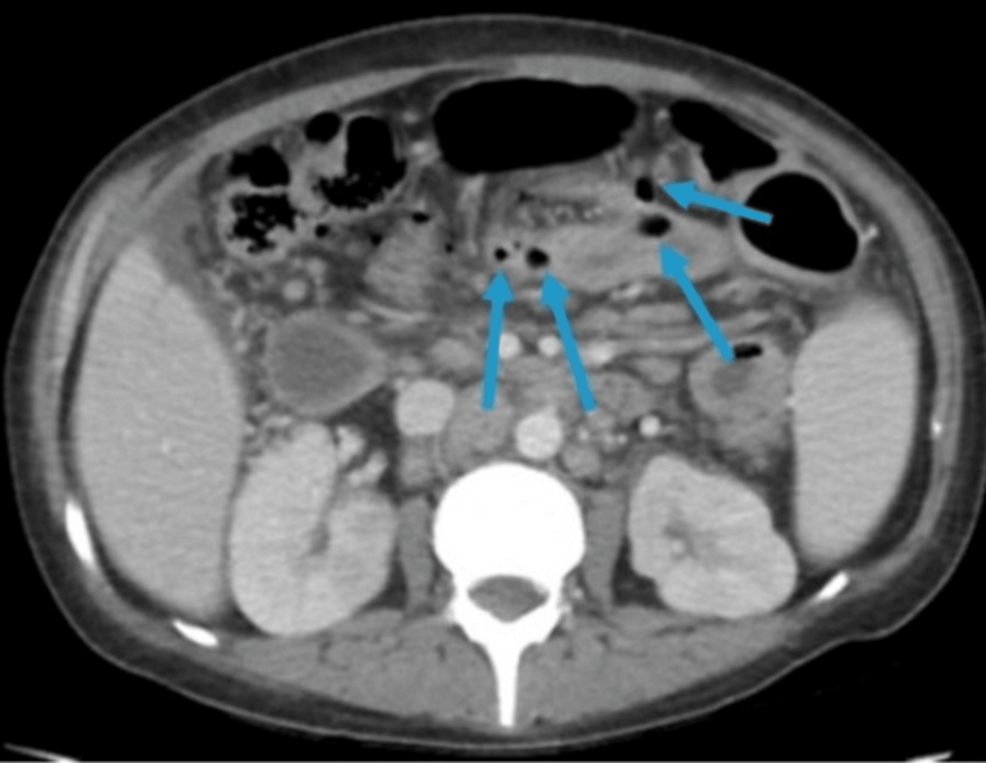
Patients were enrolled in 55 hospitals in China. They were stratified by number of prior lines of platinum-based treatment, ECOG performance status of 0 vs 1, and presence/absence of liver metastases.
Of 522 patients who were screened, 386 were randomly assigned on a 1:1 basis with 191 receiving 2.5 mg/kg iza-bren on days 1 and 8 of a 3-week cycle with 195 receiving physician’s choice of chemotherapy.1
The median age of patients was 50.0 in the treatment arm and 49.0 in the chemotherapy arm, with the majority being male in each arm (85.3% and 81.0%, respectively). The majority had ECOG performance status of 1 (75.9% in both arms). Over half of patients in both arms had received 2 prior lines of therapy with the rest having received at least 3 lines. The majority had received 2 prior lines of chemotherapy, with 48.2% of each arm having received 2 prior lines of platinum-based chemotherapy. Prior radiotherapy had been used in 89.5% of the experimental arm and 88.2% of the control arm.
Metastases were present at baseline in the liver, bones, and lungs in 47.6%, 49.2%, and 46.6% of the experimental arm and 48.7%, 46.7%, and 37.4% of the control arm.
Results were reported at median follow-up of 7.66 months for iza-bren and 7.10 months for chemotherapy. There was 1 complete response in the iza-bren arm and none in the control arm. The disease control rate was 82.4% with iza-bren vs 69.6% with chemotherapy. All subgroups favored iza-bren in this analysis.
The median DOR was 8.5 months for iza-bren vs 4.8 months for physician’s choice of chemotherapy (HR, 0.43; 95% CI, 0.22–0.83). The median PFS was 8.38 months with iza-bren vs 4.34 months for chemotherapy (HR, 0.44; 95% CI, 0.32–0.62), and this trend was consistent across subgroups. At this time, OS was not mature.
Treatment-related adverse events (TRAEs) of grade 3 or higher were reported in 79.9% of patients receiving iza-bren vs 61.6% of those receiving chemotherapy. Serious TRAEs occurred in 43.4% of patients in the iza-bren arm vs 27.0% in the chemotherapy arm, and 4 (2%) treatment-related deaths occurred in the iza-bren group. Dose reductions due to TRAEs were needed in 41.8% with iza-bren vs 24.3% with chemotherapy, and TRAEs leading to dose interruption occurred in 61.4% vs 18.4%, respectively. TRAEs led to treatment discontinuation in 2.6% vs 3.2%, respectively.
Hematological AEs were reported more frequently with iza-bren vs chemotherapy including anemia in 50% vs 10% and decreased platelet count in 43% vs 7%. Decreased white blood cell count occurred in 43% vs 44% and decreased neutrophil count occurred in 38% vs 41%, respectively. According to Zhou, these were well managed by standard supportive care. The majority of nonhematologic TRAEs were grade 1 or 2, and no new safety signals were identified.
Two cases of grade 2 interstitial lung disease (ILD) occurred in the experimental arm and 2 cases of grade 3 ILD occurred in the chemotherapy arm.
“Based on this trial, iza-bren represents a potential new standard of care for heavily pretreated patients with recurrent or metastatic NPC,” concluded Zhou.