Terms
While we only use edited and approved content for Azthena
answers, it may on occasions provide incorrect responses.
Please confirm any data provided with the related suppliers or
…

Terms
While we only use edited and approved content for Azthena
answers, it may on occasions provide incorrect responses.
Please confirm any data provided with the related suppliers or
…

As announced on The Scott Mills Radio 2 Breakfast Show this morning, Madness will make their BBC Radio 2 In Concert debut with an exclusive intimate performance. The set will be recorded at the BBC Radio Theatre in London’s New Broadcasting…
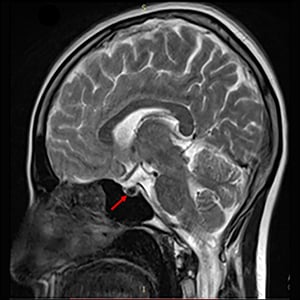
Ajeesh Thulaseedharan, Puthiyaveetil Khadar Jabbar, Sandra Mosses
JCEM Case Reports, Volume 3, Issue 10, October 2025, luaf148
https://doi.org/10.1210/jcemcr/luaf148
Hereditary hemochromatosis type 2A (juvenile hemochromatosis)…
It was derided by some critics as self-indulgent and “gimmicky” when it was released in 1975 but has since been marked a perfect 10 and inspired exhibitions and postage stamps.
Now to mark the 50th anniversary of Pink Floyd’s album Wish You…
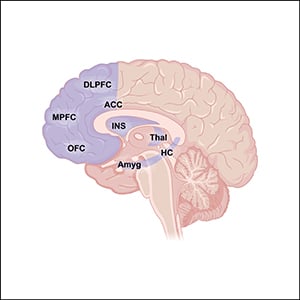
Heather Valera, Angela Chen, Kathryn J Grive
Endocrinology, Volume 166, Issue 10, October 2025, bqaf137
https://doi.org/10.1210/endocr/bqaf137
The hypothalamic-pituitary-ovarian (HPO) axis is a complex endocrine feedback…

Acute Generalized Exanthematous Pustulosis (AGEP) is a rare but severe dermatologic condition, typically characterized by the sudden onset of widespread sterile pustules on an erythematous and edematous base. Most AGEP cases are drug-induced hypersensitivity reactions, although infections and other immune-related causes have also been reported.1 Clinically, AGEP presents with rapidly developing pustular eruptions, often within 24–48 hours, accompanied by fever, pruritus, and systemic discomfort. In severe cases, disease progression may lead to skin desquamation, multi-organ involvement, and serious complications, with mortality reported in a minority of patients.2,3
The risk factors for drug-induced AGEP are multifactorial, including drug class, dosage, duration of exposure, prior sensitization, and individual immunologic susceptibility. Antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most frequently implicated agents, yet the underlying mechanisms remain incompletely understood.4 A systematic investigation into pharmacologic triggers and clinical risk factors is therefore warranted to support improved recognition and management.
The FDA Adverse Event Reporting System (FAERS) provides a large-scale pharmacovigilance platform with detailed reports on drug exposure, dosing, concomitant therapies, and clinical outcomes. Leveraging this resource allows the identification of safety signals and the evaluation of drug-specific risks associated with rare but serious adverse events such as AGEP.5
Accordingly, this study analyzed FAERS data from 2004 to 2024 to characterize drug-related risk factors for AGEP. We focused on implicated drug categories, patterns of use, and potential interactions associated with disease onset. The findings are expected to provide useful evidence for drug safety monitoring and to facilitate early identification of patients at risk.
This real-world, retrospective pharmacovigilance study was conducted using data from the FAERS, covering the period from the first quarter of 2004 to the fourth quarter of 2024. Adverse drug reactions (ADRs) related to AGEP were identified using the Medical Dictionary for Regulatory Activities (MedDRA) terminology, specifically by selecting the preferred term “Acute Generalized Exanthematous Pustulosis.”
The data were retrieved from the FAERS Public Dashboard, a web-based interface that allows users to access adverse event reports submitted by pharmaceutical companies, healthcare professionals, and consumers. Each report contains multiple variables, including the suspected drug’s active ingredient, indication for use, severity of the adverse reaction, date of event onset, patient demographics (eg, age, sex, weight), type and source of the reporter, concomitant medications, geographic location, and any associated literature references. In each report, drugs are assigned different roles in relation to the adverse event (eg, primary suspect, secondary suspect, concomitant, or interacting drug). For this analysis, only cases where the drug was designated as the “primary suspect” for AGEP were included.
Disproportionality analysis was performed using the Reporting Odds Ratio (ROR) and its corresponding 95% confidence interval (CI) to evaluate the strength of association between suspected drugs and AGEP (Tables 1 and 2). Drugs known to be used for the treatment of AGEP were excluded. A potential safety signal was considered present if the lower bound of the 95% CI for the ROR exceeded 1 and the upper bound was greater than 3.5
|
Table 1 Four Fold Table for Measures of disproportionality5
|
 |
Table 2 Formulas and Threshold Values of ROR5
|
P-adjust refers to the p-value after Fisher’s exact test and Bonferroni correction. A volcano plot was generated, with -log(p-adjust) on the x-axis and logROR on the y-axis.
Patient-level data including sex, age, and body weight were extracted from FAERS reports. Only reports with complete information were included in the analysis. Records with implausible values—defined as age over 120 years or body weight exceeding 400 kg—were excluded.
Univariate analysis was conducted for all suspected drugs. A drug was considered significant if it met the following criteria: a lower bound of the 95% confidence interval (CI) for the reporting odds ratio (ROR) greater than 1, ROR > 100, and an adjusted p-value (p-adjust) < 0.01. Drugs meeting these thresholds were then included in a Least Absolute Shrinkage and Selection Operator (LASSO) regression model for feature selection. Variables selected by the LASSO model, along with relevant patient characteristics, were subsequently included in a multivariate logistic regression to identify potential risk factors associated with drug-induced AGEP.
Baseline characteristics of drug-associated AGEP cases are summarized in Table 3 and Figure 1. Between the first quarter of 2004 and the fourth quarter of 2024, a total of 18,214,476 adverse events (AEs) were reported in the FAERS database, among which 6,880 cases were identified as AGEP. Of these, 3,750 cases (54.5%) involved female patients, 2,471 cases (35.9%) involved male patients, and 659 reports (9.6%) lacked gender information. The median age of AGEP patients was 59 years, and the median body weight was 83 kg. Notably, 39.2% (n = 2,699) of reports were submitted by healthcare professionals. France, the United States, and Spain contributed the highest number of AGEP case reports, with 1,977, 1,222, and 326 cases, respectively.
 |
Table 3 Patient Demographics
|
 |
Figure 1 Overview of reports related to drug-induced AGEP.YEAR: Number of AGEP reports submitted each year.AGE: Distribution of AGEP reports by patient age group.OUTCOME: Clinical outcomes reported in AGEP-related adverse events, Case outcomes were categorized as death (DE), life-threatening (LT), hospitalization (HO), disability (DS), congenital anomaly (CA), required intervention to prevent permanent impairment/damage (RI), and other outcomes (OT).
|
A volcano plot was generated to visualize the association between suspected drugs and AGEP (Figure 2). In this plot, the x-axis represents the logarithmic values of the reporting odds ratio (logROR), where a positive x–value indicates that adverse events associated with a given drug are reported more frequently in AGEP cases than in other adverse events. The y-axis represents the negative logarithm of the Bonferroni-adjusted p-value obtained from Fisher’s exact test, with higher values indicating stronger statistical significance. The color of each point reflects the logarithm of the number of case reports, with redder shades indicating a larger number of reports. Therefore, drugs located in the upper right quadrant of the plot are considered to have both strong association signals and high reporting frequency.
 |
Figure 2 Volcano Plot of Drugs Associated with AGEP; ROR, reporting odds ratio; P-adjust, p-value after Bonferroni correction.
|
A total of 148 drugs were found to be significantly associated with AGEP (see Supplementary Table S1). The top 10 drug classes included: antibiotics (44/148), nonsteroidal anti-inflammatory drugs (NSAIDs; 10/148), antifungals (6/148), antineoplastic agents (6/148), antiepileptics (5/148), calcium channel blockers (5/148), antituberculosis agents (4/148), contrast agents (4/148), glucocorticoids (4/148), and proton pump inhibitors (4/148).
We performed univariate analysis on suspected drugs that met the following criteria: more than 100 reported AGEP cases, ROR > 1, and both the lower bound of the 95% confidence interval and the Bonferroni-adjusted p-value < 0.01. Drugs that met these thresholds were subsequently included in the Least Absolute Shrinkage and Selection Operator (LASSO) regression model. Seventeen drugs were identified by LASSO (Figure 3) and further analyzed using multivariate logistic regression, incorporating relevant patient characteristics (Table 4).The results indicated that 17 drugs—including pantoprazole, omeprazole, terbinafine, metronidazole, ceftriaxone, and vancomycin—were significantly associated with an increased risk of AGEP. The predictive performance of the final model was evaluated using a receiver operating characteristic (ROC) curve, with an area under the curve (AUC) of 0.69 (Figure 4), indicating moderate discriminatory ability.
 |
Table 4 Results of Multivariate Logistic Regression Analysis
|
 |
Figure 3 Results of LASSO Regression Analysis,The plot shows the coefficient profiles of 17 drug variables across log(λ) values and the ten-fold cross-validation curve for λ selection using AUC as the metric, with dotted lines indicating the optimal λ values.
|
 |
Figure 4 ROC Curve for Drug-Induced AP Risk Factors;The red line represents the ROC curve for predicting the outcome, and the gray diagonal line indicates the reference line of no discrimination. The AUC was 0.690, suggesting fair discriminative ability.
|
The 17 identified risk drugs could be categorized into the following classes: antibiotics (7/17), nonsteroidal anti-inflammatory drugs (NSAIDs; 2/17), antiviral agents (3/17), proton pump inhibitors (2/17), calcium channel blockers (1/17), antifungal agents (1/17), and other (1/17).
AGEP is an acute, drug-associated cutaneous reaction characterized by the sudden onset of fever, widespread non-follicular pustular eruptions, and systemic symptoms. While its exact pathogenesis remains incompletely understood, AGEP is believed to involve drug-induced immune activation, primarily through T cell–mediated pathways that drive neutrophilic infiltration in the epidermis.6 Clinically, diagnosis relies on the hallmark skin manifestations, patient history, and histopathological confirmation. The cornerstone of management is immediate discontinuation of the culprit drug, along with symptomatic and supportive care. Although most patients recover, a subset may experience severe complications, including exfoliative dermatitis, sepsis, or multi-organ involvement, resulting in poor prognosis and mortality rates reported as high as 30%–40%.7
Previous reports have implicated various antibiotics, antiviral agents, and other commonly prescribed drugs in AGEP, but the strength of these associations has often been limited by small sample sizes or potential confounding. False-positive signals remain a concern.8 Therefore, large-scale pharmacovigilance studies are warranted to identify credible drug-related risk factors for AGEP.
In this study, we leveraged real-world data from the FAERS database to systematically analyze AGEP-related adverse event reports from 2004 to 2024. A total of 6,880 cases were identified. The majority of patients were female (54.5%) and the median age was 59 years, suggesting that AGEP predominantly affects middle-aged and older adults—a finding consistent with prior literature. This may be due to increased polypharmacy and age-related decline in immune tolerance.9 The highest number of reports originated from France, the United States, and Spain, reflecting greater pharmacovigilance activity in these regions.
Using disproportionality analysis and multivariate regression, we identified 148 drugs with significant AGEP signals, and further narrowed this list to 17 high-risk agents, spanning multiple therapeutic classes—antibiotics, NSAIDs, antivirals, proton pump inhibitors, calcium channel blockers, and antifungals.
Among the antibiotics, ceftriaxone had the highest odds ratio (OR = 49.87), highlighting its strong association with AGEP. As a third-generation cephalosporin, ceftriaxone contains a β-lactam ring that may act as a hapten, binding to host proteins and triggering IgE-mediated immediate reactions or T cell–mediated delayed hypersensitivity. Patch testing studies have shown high positivity rates for ceftriaxone among β-lactams, supporting its sensitizing potential.10 Clinical reports from Turkey and elsewhere have described rapid AGEP onset after ceftriaxone initiation, with symptoms resolving upon discontinuation.11
Metronidazole, a nitroimidazole antibiotic, may induce AGEP via aberrant immune activation. It has been shown to stimulate drug-specific CD4⁺ T cells and enhance neutrophil chemotaxis through IL-8 and GM-CSF secretion, contributing to pustule formation.12,13 Vancomycin is another well-documented trigger, and recent single-cell immunopathology studies suggest it induces a mixed immune response, including TH17-like effectors, indicating possible therapeutic targets for severe or relapsing cases.14,15
Amoxicillin and amoxicillin-clavulanate have also been frequently reported. Delayed-type T cell responses to the shared β-lactam ring structure are considered the likely mechanism, and cross-reactivity with other penicillin-class antibiotics has been demonstrated via patch testing.16,17 Clindamycin is another well-established culprit, with a median symptom resolution time of 9 days after drug withdrawal and supportive care.18,19 Although ciprofloxacin–related AGEP is rare, its potential mechanism may involve phototoxic metabolites generating free radicals under UV exposure, leading to keratinocyte damage and inflammation.20,21
Hydroxychloroquine, commonly prescribed for autoimmune diseases, has been implicated in the development of AGEP through mechanisms that may involve enhanced antigen presentation and subsequent T cell sensitization.22–24 Of particular note, a case reported by Xi’an Jiaotong University Hospital described the successful management of hydroxychloroquine-induced AGEP using secukinumab, an IL-17 pathway inhibitor, highlighting the potential role of IL-17 signaling in the pathogenesis and treatment of this condition.25
Among antiviral agents, levetiracetam, valaciclovir, and aciclovir were identified as risk drugs. Though rare, levetiracetam–related AGEP has been reported, especially when combined with other antiepileptics like valproate.26 Aciclovir and valaciclovir, used for herpesvirus infections, have been implicated in multiple AGEP cases, with rapid resolution post-withdrawal.27,28
Despite the perceived safety of proton pump inhibitors (PPIs), both pantoprazole and omeprazole were strongly associated with AGEP in this study. Case reports document typical features including pustular eruptions, fever, and leukocytosis, resolving upon discontinuation.29,30
Among NSAIDs, both ibuprofen and paracetamol were identified. While generally well-tolerated, ibuprofen has been shown to cause AGEP in rare cases.31 Though paracetamol is often considered to have low allergenic potential, there are reports of AGEP even in children, with eosinophilia and neutrophilic pustules.32
In addition, terbinafine, a systemic antifungal, was associated with AGEP, possibly due to its intracellular accumulation in keratinocytes and subsequent T cell–mediated cytotoxicity.33,34 One case demonstrated progression despite corticosteroids and eventual improvement with adalimumab therapy.35 Lastly, diltiazem, a calcium channel blocker used for hypertension and arrhythmia, has also been reported to cause AGEP with rapid onset and resolution following corticosteroid treatment.36
This study leveraged a large-scale real-world dataset from the FAERS spanning two decades (2004–2024), providing a comprehensive and representative overview of drug-induced AGEP in clinical practice. The robustness and external validity of the findings are supported by the breadth of data and diversity of reporting sources across countries. By integrating multiple statistical methods—including reporting odds ratios, univariate analysis, LASSO regression, and multivariate logistic regression—the study effectively combined signal detection, variable selection, and risk quantification. These complementary approaches enabled us to systematically identify and validate key drug-related risk factors for AGEP. A total of 148 drugs with significant associations were screened, with 17 identified as risk factors, providing clinicians with practical insights for risk-aware prescribing and targeted monitoring.
Despite these strengths, several limitations should be acknowledged. First, the FAERS database is based on spontaneous and voluntary reporting, which may introduce underreporting or selective reporting biases. Second, the completeness and granularity of clinical data in FAERS are often limited; missing values for variables such as age, body weight, and comorbidities could affect the precision and interpretability of the analysis. Third, although multivariate logistic regression was used to control for confounding, residual confounding from unmeasured variables cannot be fully excluded. It is also important to note that disproportionality analysis and FAERS data, by nature, do not allow for the establishment of causality or the estimation of incidence rates.
This study utilized real-world data from the FAERS database between 2004 and 2024 to systematically evaluate potential risk factors for drug-induced AGEP. A range of commonly prescribed medications—including antibiotics, nonsteroidal anti-inflammatory drugs (NSAIDs), antiviral agents, proton pump inhibitors, calcium channel blockers, and antifungal drugs—were found to be significantly associated with AGEP. Notably, ceftriaxone, pantoprazole, hydroxychloroquine, and vancomycin exhibited particularly high odds ratios, underscoring the need for heightened pharmacovigilance and risk assessment during their clinical use. Furthermore, the observation that AGEP was more frequent in younger and middle-aged adults suggests a possible age-related component in disease susceptibility.
Although this study employed large-scale signal detection and multivariate modeling to enhance the robustness of its findings, several limitations remain. These include the passive nature of FAERS reporting, missing clinical data, and the inability to infer causality from spontaneous reports. Therefore, future research should integrate prospective clinical studies and mechanistic investigations to elucidate the immunological basis and individual susceptibility to AGEP. Such efforts will be essential for advancing early recognition, targeted prevention, and safe prescribing practices in clinical pharmacology and dermatovigilance.
The dataset generated and analyzed during the current study is available from the corresponding authors upon reasonable request: Wanchun Wang or Xiaojian Li.
In accordance with Article 32 of the Measures for Ethical Review of Life Science and Medical Research Involving Human Beings issued by the National Science and Technology Ethics Committee of the People’s Republic of China, this study was exempted from ethical review because the data analyzed pose no harm to human participants, do not involve sensitive personal information or commercial interests, and were obtained from open and legally accessible databases.
The authors affirm that they have no commercial or financial affiliations that could be perceived as potential conflicts of interest. This includes any relationships or financial interests that could influence or bias the study’s results and conclusions.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
This research was funded by the Technology Innovation Team of Jiangxi University of Traditional Chinese Medicine (CXTD220090), National Natural Science Foundation of China Regional Projects (No. 81960874, 82260935, 82260937), Jiangxi Provincial Natural Science Foundation Key Projects (NO. 20202ACB206010).
The authors declare no conflicts of interest.
1. Szatkowski J, Schwartz RA. Acute generalized exanthematous pustulosis (AGEP): a review and update. J Am Acad Dermatol. 2015;73(5):843–848. doi:10.1016/j.jaad.2015.07.017
2. Parisi R, Shah H, Navarini AA, et al. Acute Generalized Exanthematous Pustulosis: clinical Features, Differential Diagnosis, and Management. Am J Clin Dermatol. 2023;24(4):557–575. doi:10.1007/s40257-023-00779-3
3. Sussman M, Napodano A, Huang S, Are A, Hsu S, Motaparthi K. Pustular Psoriasis and Acute Generalized Exanthematous Pustulosis. Medicina. 2021;57(10):1004. doi:10.3390/medicina57101004
4. de Groot AC. Results of patch testing in acute generalized exanthematous pustulosis (AGEP): a literature review. Contact Dermatitis. 2022;87(2):119–141. doi:10.1111/cod.14075
5. Li X, Yan Z, Chen S, Wu Y, Qiu G, Hu F. Potential drugs associated with toxic epidermal necrolysis: a disproportionality analysis based on the FAERS database (2004–2024). Arch Dermatol Res. 2025;317(1):647. doi:10.1007/s00403-025-04107-z
6. Demircioğlu D, Karabıyık N, Durmaz EÖ, Demirkesen C, Şahin S. AGEP sine pustulosis induced by hydroxychloroquine used for COVID-19 infection. Dermatol Ther. 2022;35(3):e15263. doi:10.1111/dth.15263
7. Stadler PC, Oschmann A, Kerl-French K, et al. Acute Generalized Exanthematous Pustulosis: clinical Characteristics, Pathogenesis, and Management. Dermatology. 2023;239(3):328–333. doi:10.1159/000529218
8. Campanón-Toro MV, Sierra O, Moreno E, Sobrino-García M, Gracia-Bara MT, Dávila I. Acute generalized exanthematous pustulosis (AGEP) induced by azithromycin. Contact Dermatitis. 2017;76(6):363–364. doi:10.1111/cod.12717
9. Pezzarossa E, Ungari M, Caresana G, et al. Acute Generalized Exanthematous Pustulosis (AGEP) in 12 Patients Treated for SARS-CoV-2 Positive Pneumonia. Am J Dermatopathol. 2021;43(5):342–348. doi:10.1097/DAD.0000000000001819
10. Stingeni L, Francisci D, Bianchi L, et al. Severe adverse drug reaction in SARS-CoV-2 infection: AGEP induced by ceftriaxone and confirmed by patch test. Contact Dermatitis. 2021;85(3):366–368. doi:10.1111/cod.13857
11. Nacaroglu HT, Celegen M, Ozek G, et al. Acute generalized exanthematous pustulosis induced by ceftriaxone use. Postepy Dermatol Alergol. 2014;4(4):269–271. doi:10.5114/pdia.2014.40938
12. Qulu WP, Mzobe G, Mtshali A, et al. Metronidazole Treatment Failure and Persistent BV Lead to Increased Frequencies of Activated T- and Dendritic-Cell Subsets. Microorganisms. 2023;11(11):2643. doi:10.3390/microorganisms11112643
13. Kostaki M, Polydorou D, Adamou E, Chasapi V, Antoniou C, Stratigos A. Acute localized exanthematous pustulosis due to metronidazole. J Eur Acad Dermatol Venereol. 2019;33(3):e109–e111. doi:10.1111/jdv.15274
14. Dellatorre Diniz B, Poudel D, Mersfelder T, Driscoll R. Vancomycin-induced acute generalised exanthematous pustulosis. BMJ Case Rep. 2025;18(1):e263634. doi:10.1136/bcr-2024-263634
15. Mukherjee EM, Gibson A, Krantz MS, et al. Single-cell immunopathology of recurrent acute generalized exanthematous pustulosis associated with vancomycin. J Allergy Clin Immunol Glob. 2025;4(2):100426. doi:10.1016/j.jacig.2025.100426
16. Bomarrito L, Zisa G, Delrosso G, Farinelli P, Galimberti M. A case of acute generalized exanthematous pustulosis due to amoxicillin-clavulanate with multiple positivity to beta-lactam patch testing. Eur Ann Allergy Clin Immunol. 2013;45(5):178–180.
17. Gaibino N, Bigotte Vieira M, Filipe P, Oliveira A. Acute generalised exanthematous pustulosis due to amoxicillin-clavulanate. BMJ Case Rep. 2016;2016:bcr2015213839. doi:10.1136/bcr-2015-213839
18. Aiempanakit K, Apinantriyo B. Clindamycin-induced acute generalized exanthematous pustulosis: a case report. Medicine. 2020;99(21):e20389. doi:10.1097/MD.0000000000020389
19. Smeets TJ, Jessurun N, Härmark L, Kardaun SH. Clindamycin-induced acute generalised exanthematous pustulosis: five cases and a review of the literature. Neth J Med. 2016;74(10):421–428.
20. Foti C, Romita P, Zanframundo G, et al. Ciprofloxacin induced acute generallised exanthematous pustulosis. Indian J Pharmacol. 2017;49(1):119–120. doi:10.4103/0253-7613.201014
21. Hausermann P, Scherer K, Weber M, Bircher AJ. Ciprofloxacin-induced acute generalized exanthematous pustulosis mimicking bullous drug eruption confirmed by a positive patch test. Dermatology. 2005;211(3):277–280. doi:10.1159/000087024
22. Ponticelli C, Moroni G. Hydroxychloroquine in systemic lupus erythematosus (SLE). Expert Opin Drug Saf. 2017;16(3):411–419. doi:10.1080/14740338.2017.1269168
23. Mercogliano C, Khan M, Lin C, Mohanty E, Zimmerman R. AGEP overlap induced by hydroxychloroquine: a case report and literature review. J Community Hosp Intern Med Perspect. 2018;8(6):360–362. doi:10.1080/20009666.2018.1547089
24. Zheng Q, Jin N, Cheng H. Hydroxychloroquine-induced acute generalized exanthematous pustulosis with HLA-typing. Pharmacogenomics. 2024;25(14–15):569–572. doi:10.1080/14622416.2024.2430167
25. Wang Y, Liu Y, Feng C, Wang M, Wang Q, Geng S. Hydroxychloroquine-induced acute generalized exanthematous pustulosis (AGEP) treated with secukinumab. J Eur Acad Dermatol Venereol. 2024;38(9):e769–e771. doi:10.1111/jdv.19875
26. Levy ZD, Slowey M, Schulder M. Acute generalized exanthematous pustulosis secondary to levetiracetam and valproic acid use. Am J Emerg Med. 2017;35(7):1036. doi:10.1016/j.ajem.2017.02.017
27. Kubin ME, Jackson P, Riekki R. Acute Generalized Exanthematous Pustulosis Secondary to Acyclovir Confirmed by Positive Patch Testing. Acta Derm Venereol. 2016;96(6):860–861. doi:10.2340/00015555-2352
28. Mao K, Li J, Zhu X, Sun H, Zhong S, Mao W. Signal mining study of severe cutaneous adverse events of valaciclovir or Acyclovir based on the FAERS database. Expert Rev Clin Pharmacol. 2024;17(1):101–110. doi:10.1080/17512433.2023.2294002
29. Schmitz B, Sorrells T, Glass JS. Acute generalized exanthematous pustulosis caused by pantoprazole. Cutis. 2018;101(5):E22–E23.
30. Nantes Castillejo O, Zozaya Urmeneta JM, Valcayo Peñalba A, Martínez-Peñuela Virseda JM. Pustulosis exantemática aguda generalizada inducida por omeprazol [Acute generalized exanthematous pustulosis induced by omeprazole]. Gastroenterol Hepatol. 2008;31(5):295–298. doi:10.1157/13119883
31. Belz D, Persa OD, Haese S, Hunzelmann N. Acute generalized exanthematous pustulosis caused by ibuprofen-Diagnosis confirmed by patch testing. Contact Dermatitis. 2018;79(1):40–41. doi:10.1111/cod.12978
32. Lapeere H, Aben A, Willekens J. Acute generalized exanthematous pustulosis following paracetamol ingestion in a 5-year-old child: a case report. Contact Dermatitis. 2022;87(3):290–291. doi:10.1111/cod.14140
33. Correia B, Costa J, Egipto P, Reis P. Terbinafine-Induced Acute Generalized Exanthematous Pustulosis. J Burn Care Res. 2021;42(4):829–831. doi:10.1093/jbcr/irab023
34. de Oliveira GV, Maia MLP, Leão FAA, et al. What to expect when AGEP is induced by terbinafine? Case report and critical review of the literature. Mycoses. 2022;65(10):918–925. doi:10.1111/myc.13506
35. Deng L, He B, Ali K, Bu Z. Terbinafine Induced Acute Generalized Exanthematous Pustulosis Treated with Adalimumab: recalcitrant to Systemic Corticosteroid Therapy. Clin Cosmet Invest Dermatol. 2023;16:9–15. doi:10.2147/CCID.S391979
36. Bangolo AI, Yelton-Torres K, Mahajan A, et al. A Case of Diltiazem-Induced Pustular Rash in an 83-Year-Old Female. Case Rep Dermatol Med. 2024;2024:9547206. doi:10.1155/2024/9547206

Benz Hui, a veteran Hong Kong performer dubbed the “King of Suppporting Actors” during a career which spanned more than five decades, has died at the age of 76.
He passed away in the early hours of Tuesday at a hospital in Hong Kong after…

Acinetobacter baumannii, a Gram-negative opportunistic pathogen, is a leading cause of hospital-acquired infections, frequently implicated in ventilator-associated pneumonia, bloodstream infections, and severe post-traumatic…