Neoadjuvant treatment with fam-trastuzumab deruxtecan-nxki (T-DXd; Enhertu) followed by paclitaxel, trastuzumab (Herceptin), and pertuzumab (Perjeta; THP) led to an improvement in pathologic complete response (pCR) rate compared with dose-dense doxorubicin and cyclophosphamide plus THP (ddAC-THP) in patients with high-risk, HER2-positive early breast cancer, according to data from the phase 3 DESTINY-Breast11 trial (NCT05113251).1
Findings presented at the 2025 ESMO Congress demonstrated that patients treated with T-DXd followed by THP (n = 321) experienced a pCR rate of 67.3% compared with 56.3% for those given ddAC-THP (n = 320; difference, 11.2%; 95% CI, 4.0%-18.3%; P = .003). Notably, the pCR benefit was observed in the hormone receptor–positive population, where the pCR rate was 61.4% in the T-DXd arm (n = 236) vs 52.3% in the ddAC-THP arm (n = 235; difference, 9.1%; 95% CI, 0.2%-17.9%), as well as the hormone receptor–negative population, where the respective pCR rates for the T-DXd arm (n = 83) and ddAC-THP arm (n = 85) were 83.1% and 67.1% (difference, 16.1%; 95% CI, 3.0%-28.8%).
“DESTINY-Breast11 showed the highest reported pCR rate in HER2-positive early breast cancer for a registrational study in the neoadjuvant setting, despite—if you want to do cross-trial comparisons—a high prevalence of hormone receptor–positive disease and a high-risk population,” lead study author Nadia Harbeck, MD, PhD, said in a presentation of the data.
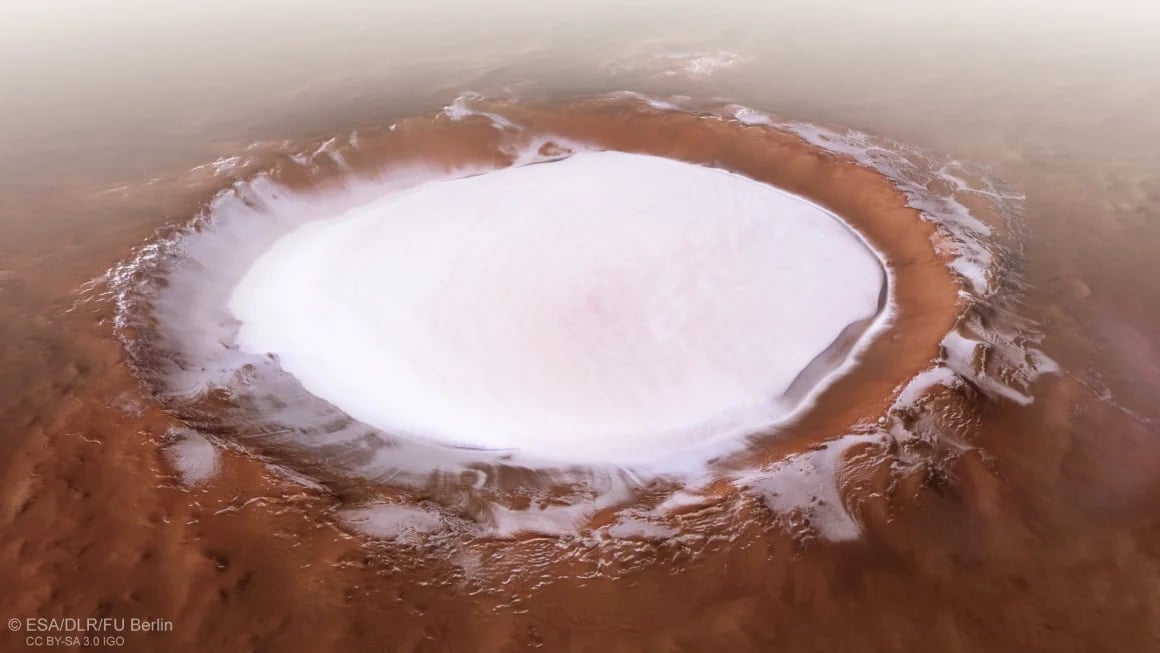
DestinyBreast-11 Highlights
- Neoadjuvant T-DXd followed by THP generated a pCR benefit vs ddAC-THP in patients with high-risk, HER2-positive early breast cancer, with the experimental regimen generating an 11.2% pCR rate improvement.
- The FDA is reviewing a supplemental biologics license application seeking the approval of neoadjuvant T-DXd plus THP in this patient population.
- The T-DXd monotherapy arm in DESTINY-Breast11 was closed early following a recommendation from the trial’s independent data monitoring committee.
Harbeck is director of the Breast Center and chair for Conservative Oncology at the Department of OB&GYN at LMU University Hospital in Munich, Germany.
How Was the DESTINY-Breast11 Trial Designed?
Harbeck noted that current neoadjuvant standard-of-care (SOC) regimens for HER2-positive early breast cancer have remained unchanged for more than a decade. As such, investigators sought to evaluate T-DXd–based treatment in this population with the goal of improving efficacy and safety vs the current SOC.
The randomized, global, multicenter, open-label study enrolled patients with previously untreated HER2-positive early breast cancer who had high-risk disease, defined as ≥cT3 and N0-3 or cT0-4 and N1-3; or inflammatory breast cancer. Patients were allowed to enroll, irrespective of hormone receptor status.
Patients were randomly assigned in a 1:1:1 fashion to receive T-DXd followed by THP; ddAC-THP; or T-DXd alone, followed by surgery in all arms. In the first arm, patients received 4 cycles of T-DXd followed by 4 cycles of THP. In the second, ddAC was administered for 4 cycles, followed by 4 cycles of THP. In the final arm, patients received T-DXd alone for 8 cycles.
Notably, the T-DXd monotherapy arm was closed in March 2024, following a recommendation from the study’s independent data monitoring committee.
After surgery, study protocols called for the following treatments, irrespective of arm:
- pCR: radiotherapy and concomitant trastuzumab with or without pertuzumab for up to 1 year
- Non-pCR: radiotherapy and ado-trastuzumab emtansine (Kadcyla) for up to 14 cycles
- Hormone receptor–positive disease: endocrine therapy
The study’s primary end point was pCR rate (ypT0/Tis ypN0) per blinded independent central review (BICR) assessment. Secondary end points included BICR-assessed pCR rate (ypT0 ypN0), event-free survival (EFS), safety, pharmacokinetics, invasive disease-free survival, overall survival, and health-related quality of life. Residual cancer burden (RCB) was an additional outcome measured during the study.
At data cutoff, 16.9% of patients in the T-DXd plus THP arm discontinued a study drug, including T-DXd (2.8%), paclitaxel (14.4%), trastuzumab (2.2%), and pertuzumab (2.2%); 97.2% of patients in this arm proceeded to surgery. In the ddAC-THP arm, 13.8% of patients had discontinued any study treatment, including AC (2.9%), paclitaxel (12.0%), trastuzumab (3.0%), and pertuzumab (3.7%); 93.8% of patients in this arm underwent surgery. In the T-DXd monotherapy arm (n = 286), 18.4% of patients discontinued study treatment, and 95.8% underwent surgery.
Regarding post-neoadjuvant treatments, 99.1% of evaluable patients in the T-DXd arm who achieved a pCR (n = 226) underwent any adjuvant therapy, comprising any cytotoxic chemotherapy regimen (5.8%), any T-DM1–containing regimen (1.8%), and any trastuzumab-containing regimen (94.2%). In the ddAC-THP, 98.4% of patients who achieved a pCR (n = 190) underwent any adjuvant therapy, including any cytotoxic chemotherapy regimen (5.8%), any T-DM1–containing regimen (2.1%), and any trastuzumab-containing regimen (91.6%).
For patients who did not achieve a pCR, any adjuvant therapy was administered to 89.5% of patients in the T-DXd plus THP arm (n = 95) and 82.3% of patients in the ddAC-THP arm (n = 130). In the experimental group, adjuvant therapies included any cytotoxic chemotherapy regimen (10.5%), any T-DM1–containing regimen (52.6%), and any trastuzumab-containing regimen (38.9%). These respective rates were 9.2%, 56.9%, and 26.2% in the control group.
In the T-DXd plus THP and ddAC-THP arms, the median age was 50 years (range, 25-82) and 50 years (range, 23-79), respectively. All patients in both arms were female. The highest proportion of patients in each arm was from Asia (T-DXd plus THP, 47.4%; ddAC-THP, 47.5%) and were Asian (49.8%; 49.1%). Most patients had an ECOG performance status of 0 (86.6%; 87.5%), had immunohistochemistry 3+ HER2-positive disease (87.2%; 88.4%), had cT0-2 tumors (54.8%; 58.8%), and had positive lymph nodes (89.4%; 87.8%).
What Were the Other Efficacy Outcomes for T-DXd Plus THP vs ddAC-THP?
Findings also showed that 81.3% of patients in the T-DXd plus THP arm had no RCB (RCB-0) or minimal RCB (RCB-1) in resected breast or lymph node tissue compared with 69.1% in the ddAC-THP arm (difference, 12.2%). In the hormone receptor–positive population, the RCB-0 plus RCB-1 rates were 78.0% for T-DXd plus THP vs 64.7% for ddAC-THP; these respective rates were 90.4% and 81.2% in the hormone receptor–negative population.
Investigators also reported an EFS trend favoring T-DXd plus THP, with data at 4.5% maturity (HR, 0.56; 95% CI, 0.26-1.17). Maturity for the data cutoff of the trial’s final analysis is predicted at approximately 10%. The 24-month EFS rates were 96.9% (95% CI, 93.5%-98.6%) in the T-DXd plus THP arm vs 93.1% (95% CI, 88.7%-95.8%) in the ddAC-THP arm.
What Is the Safety Profile of T-DXd Plus THP?
Any-grade adverse effects (AEs) occurred in 98.1% of patients in the T-DXd plus THP arm compared with 98.7% of patients in the ddAC-THP arm. The respective rates of grade 3 or higher AEs were 37.5% and 55.8%. Any-grade serious AEs were reported in 10.6% and 20.2% of patients, respectively.
In the T-DXd plus THP arm, AEs led to dose any dose reduction, any drug interruption, and any treatment discontinuation in 18.1%, 37.8%, and 14.1% of patients, respectively. In the ddAC-THP group, these rates were 19.2%, 54.5%, and 9.9%, respectively. AEs led to death in 0.6% of patients in both arms. AEs led to delays in surgery in 3.4% of patients in the experimental arm vs 2.6% of patients in the control arm.
Regarding AEs of special interest, any-grade drug-related adjudicated interstitial lung disease (ILD) was 4.4% in the T-DXd plus THP arm vs 5.1% in the ddAC-THP arm. The rates of grade 3 or higher ILD were 0.6% and 1.9%, respectively. Grade 5 ILD occurred in 1 patient (0.3%) in both groups. Any-grade left ventricular dysfunction occurred in 1.3% of patients in the experimental arm vs 6.1% of patients in the control arm. The rates of grade 3 or higher left ventricular dysfunction were 0.3% and 1.9%, respectively, although no grade 5 events were reported in either group.
Any-grade treatment-emergent AEs reported in at least 20% of patients in either arm included nausea (T-DXd plus THP, 64.7%; ddAC-THP, 51.6%), diarrhea (58.8%; 54.2%), alopecia (47.5%; 49.0%), fatigue (41.3%; 54.8%), increased transaminase levels (34.4%; 33.7%), neutropenia (29.1%; 44.2%), constipation (29.1%; 24.4%), vomiting (28.8%; 21.2%), peripheral neuropathy (25.9%; 20.8%), anemia (22.8%; 49.7%), stomatitis (18.4%; 27.9%), and leukopenia (17.2%; 23.4%).
What Data Were Reported for T-DXd Monotherapy in HER2+ Early Breast Cancer?
When the T-DXd monotherapy arm, patients were allowed to remain on therapy or immediately switch to local SOC. If patients switched therapy, they were classified as having a non-pCR.
Findings from the monotherapy arm showed that patients (n = 286) achieved a pCR rate of 43.0% at the primary analysis and 51.4% at a prespecified supplementary analysis. EFS data were similar between T-DXd monotherapy and ddAC-THP (HR, 0.82; 95% CI, 0.41-1.62), and the 24-month EFS rate in the T-DXd monotherapy group was 94.4% (95% CI, 90.5%-98.7%).
Regarding safety, 97.5% of patients treated with T-DXd alone (n = 283) experienced any-grade AEs, 22.6% had grade 3 or higher AEs, and 10.2% had any-grade serious AEs. AEs led to dose reduction, drug interruption, and treatment discontinuation in 6.7%, 18.0%, and 7.8% of patients, respectively. One patient (0.4%) experienced an AE that led to death. AEs led to surgical delay in 6.4% of patients.
The rate of any-grade, drug-related adjudicated ILD was 4.9% in the T-DXd monotherapy arm, although all instances were grade 1 or 2. Left ventricular dysfunction occurred in 0.7% of patients, all at grade 1 or 2.
What’s Next for T-DXd Plus THP?
Based on data from DESTINY-Breast11, the FDA accepted a supplemental biologics license application seeking the approval of neoadjuvant T-DXd followed THP for the treatment of adult patients with high-risk, HER2-positive (IHC 3+ or in situ hybridization–positive), stage II/III breast cancer.2
The FDA has assigned a target action date of May 18, 2026, under the Prescription Drug User Fee Act.
“DESTINY-Breast11 results support T-DXd [plus] THP as a more effective and less toxic neoadjuvant treatment compared with ddAC-THP, and it may become the preferred regimen for patients with high-risk, HER2-positive early breast cancer,” Harbeck concluded in her presentation.1
Disclosures: Harbeck reported receiving honoraria from AstraZeneca, Daiichi Sankyo, Gilead, Lilly, Menarini Stemline, MSD, Novartis, Pfizer, Pierre Fabre, Roche, Viatris, and Zuellig Pharma; serving as a consultant or advisor for Exact Sciences, Gilead, Pfizer, Roche, and Sandoz; having an institutional site contract with AstraZeneca; serving as a data safety monitoring board or advisory board member for Gilead, IQVIA, and Roche; and having ownership interested in the West German Study Group.
References
- Harbeck N, Modi S, Pusztai L, et al. DESTINY-Breast11: neoadjuvant trastuzumab deruxtecan alone (T-DXd) or followed by paclitaxel + trastuzumab + pertuzumab (T-DXd-THP) vs SOC for high-risk HER2+ early breast cancer (eBC). Presented at: 2025 ESMO Congress; October 17-21, 2025; Berlin, Germany. Abstract 291O.
- Enhertu followed by THP supplemental biologics license application accepted in the U.S. for patients with high-risk HER2 positive early-stage breast cancer prior to surgery. News release. Daiichi Sankyo. October 1, 2025. Accessed October 18, 2025. https://www.daiichisankyo.com/files/news/pressrelease/pdf/202510/20251001_E.pdf