Introduction
Mortality related to severe pneumonia exceeds 30% among immunocompromised patients admitted to ICUs,1 largely attributable to delayed pathogen identification and inappropriate antimicrobial therapy.2 Legionella pneumophila (L. pneumophila), an elusive respiratory pathogen, exemplifies this diagnostic dilemma, accounting for 1%–10% of community-acquired pneumonia (CAP) with rapid progression to respiratory failure and multi-organ dysfunction.3 Approximately 44% of patients require intensive care, with mortality rates of 10%–15% that rise to 25%–50% in nosocomial settings.3 Misdiagnosis frequently leads to delayed or inappropriate therapy and unnecessary broad-spectrum antibiotic use, exacerbating both mortality risk and antimicrobial resistance.
This fastidious gram-negative bacterium evades routine culture4 and presents nonspecifically.5 Hyponatremia and extrapulmonary symptoms may provide clues, but definitive diagnosis traditionally relies on urinary antigen testing (limited to serogroup 1) or retrospective serology (delayed antibody response).6 Although these methods retain useful in stable, community-acquired pneumonia or epidemiological surveillance due to their rapidity and cost-effectiveness, they are suboptimal for guiding initial therapy in critically ill immunocompromised hosts, in whom a broad range of pathogens must be rapidly ruled out. This diagnostic delay is particularly consequential in high-risk populations, such as patients with renal failure, diabetes, or immunosuppression, where mortality can reach 80% without targeted treatment.2
Molecular diagnostics have emerged as promising tools to address these gaps. Pathogen-targeted PCR assays deliver results within hours but cover limited pathogen panels.7 Metagenomic next-generation sequencing (mNGS) enables hypothesis-free detection of all nucleic acids in clinical samples, yet its quantitative accuracy may be compromised by host DNA dominance or low pathogen biomass.8 Digital PCR (dPCR) provides absolute quantification of pathogen load but suffers from low throughput.9 Isothermal amplification technology, as one of the best candidates for replacing with PCR method, is also gradually being applied in the field of rapid pathogen detection.10 While individual technologies demonstrate advantages, evidence supporting their synergistic application for diagnosing rare pathogens like Legionella remains scarce.
The COVID-19 pandemic has further complicated pneumonia management. Immunosuppressive therapies used in severe cases (eg corticosteroids) increase susceptibility to opportunistic infections, including Legionella and fungi.2 This creates a critical need for rapid, comprehensive diagnostic strategies that differentiate viral, bacterial, and fungal co-infections to guide precision therapy.
Here, we present a clinically instructive case of severe pneumonia in an immunocompromised host, where an integrated molecular approach incorporating isothermal amplification, dPCR, and mNGS enabled rapid confirmation of L. pneumophila with concurrent Candida glabrata coinfection. This case yields three pivotal insights: (1) Technical synergy: Initial isothermal amplification delivered pathogen-specific positivity within 12 hours; subsequent dPCR overcame false negativity via sample dilution, confirming nucleic acid inhibition; while mNGS independently validated Legionella and uncovered fungal co-infection. (2) Therapeutic precision: Molecular diagnostics facilitated prompt transition from empirical antibiotics to targeted anti-legionella (fluoroquinolone/macrolide) and antifungal therapy (amphotericin B), with serial PCT/CRP trends objectively tracking therapeutic response. (3) Clinical impact: The 72-hour diagnostic pathway outperformed conventional methods, potentially reducing mortality risk by 3-fold versus traditional culture-dependent approaches.
This report underscores the viability of integrated molecular diagnostics as a new standard for critical pneumonia in immunocompromised hosts, directly informing antimicrobial stewardship and improving outcomes in complex co-infections.
Case Presentation
A 57-year-old female with a complex medical history presented to the emergency department on September 7, 2024, with acute dyspnea exacerbation over 2 hours. Her comorbidities included: Rheumatic heart disease (mechanical valve replacement, 2018), Chronic renal failure (CKD stage 4, eGFR 22 mL/min/1.73m²), Type 2 diabetes mellitus (HbA1c 8.6%), Chronic nephritic syndrome on immunosuppressive therapy (prednisone 10 mg/day). Vital signs upon admission included temperature 37.8°C, heart rate 110 bpm (atrial fibrillation), respiratory rate 28 breaths/min, SpO2 88% on room air. Physical examination revealed bilateral basal crackles and pedal edema.
Initial Diagnostic Investigations
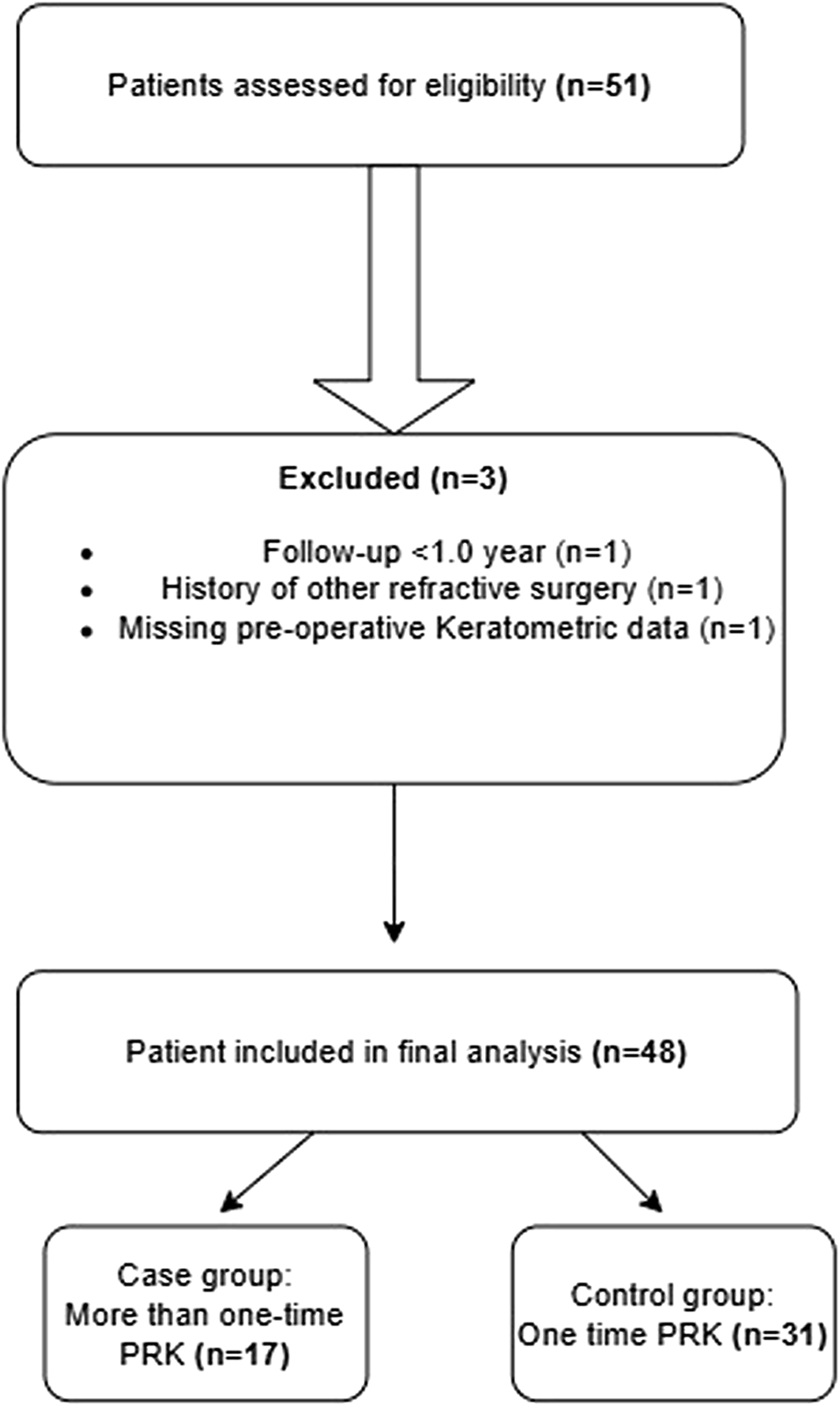
Laboratory findings demonstrated leukocytosis (WBC 19.03 × 109/L, neutrophils 89%), hyponatremia (Na+ 127 mmol/L), elevated inflammatory markers (PCT 42.55 ng/mL, CRP 12.2 mg/L), and renal impairment (creatinine 265 μmol/L, BUN 31.2 mmol/L). High-resolution CT showed bilateral multifocal consolidations with ground-glass opacities and interlobular septal thickening on admission day (Figure 1A), which further progressed to diffuse patchy ground-glass opacities by day 5 (Figure 1B), collectively suggestive of severe pneumonia with interstitial involvement.
|
Figure 1 Radiological images of high-resolution chest CT. (A) Chest CT at admission showing bilateral multifocal consolidations with ground-glass opacities and interlobular septal thickening; (B) Chest CT on day 5 demonstrating a diffuse progression of patchy ground-glass opacities; (C) Chest CT on day 20 showed >70% resolution of consolidations.
|
Molecular Diagnostic Cascade
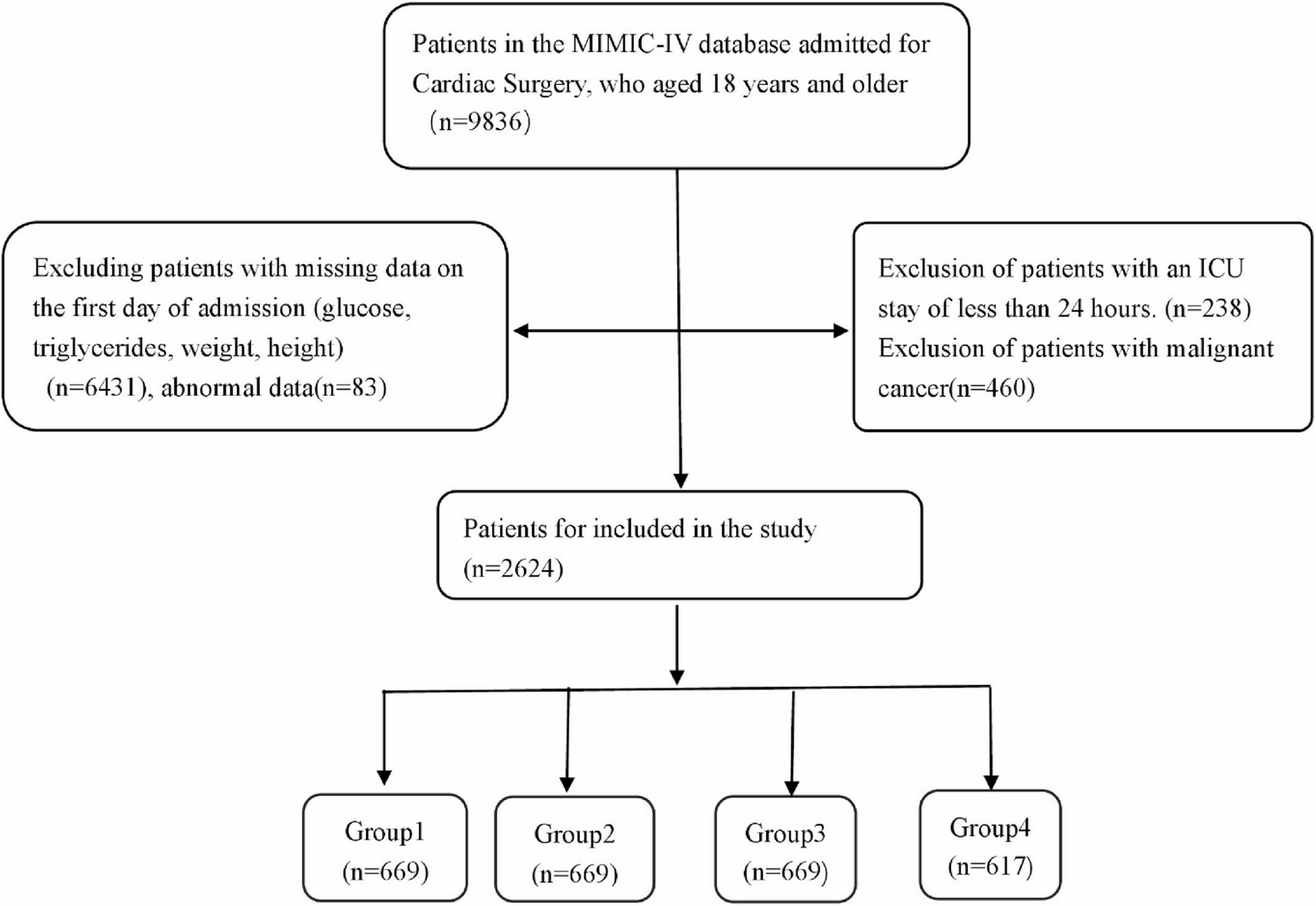
On Day 1 (ICU admission), empirical Imipenem-cilastatin (0.5g q12h, renal-adjusted) was initiated. Sputum samples were immediately subjected to respiratory pathogen panel testing via isothermal amplification (Isothermal Amplification on Disk Chip, CapitalBio Technology (Chengdu) Co., Ltd)., screening for 9 common (Streptococcus pneumoniae, Staphylococcus aureus, Methicillin-Resistant Staphylococcus aureus, Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, Stenotrophomonas maltophilia, Haemophilus influenzae and Escherichia coli) and 5 atypical (Mycobacterium tuberculosis complex, Mycoplasma pneumoniae, Chlamydophila pneumoniae and Legionella pneumophila) pathogens associated with respiratory infections (Respiratory Pathogens Nucleic Acid Detection Kit). Positive result of L. pneumophila was reported 4 hours after sample delivered to laboratory (Figure 2A). Bronchoalveolar lavage fluid (BALF) collected on Day 2 underwent comprehensive testing. dPCR (Digital PCR Assay Kit, Pilot Gene Technology, Hangzhou) of undiluted sample yielded negative results (Figure 2B); 10-fold dilution demonstrated 4,455 copies/mL of L. pneumophila (Figure 2C), indicating that high-concentration nucleic acids can inhibit amplification reactions. On Day 3, mNGS (IDseqTM Ultra, Vision Medicals, Guangzhou) revealed L. pneumophila dominance (384,661 reads, 92.7% relative abundance, Figure 2D) with concurrent Candida glabrata (C. glabrata) coinfection (3,473 reads, 80.6% relative abundance, Figure 2E). An evolution to Mixed Infection and therapeutic challenges were on Day 6 due to recurrent fever (39.2°C) with CRP rebound (↑153.4 mg/L from 96.8 mg/L), with BALF biomarkers β-D-glucan 674.8 pg/mL (normal <80). Sputum culture also confirmed fungal coinfection with Candida glabrata (>105 CFU/mL, Figure 2F).
 |
Figure 2 Multi-Platform Pathogen Diagnostic Results. (A) Isothermal amplification curves of BALF; Results of dPCR from undiluted (B) and 10-fold diluted (C) BALF; BALF mNGS gene sequence coverage depth map for Legionella pneumophila (D) and Candida glabrata (E); (F) Candida glabrata colonies from sputum culture.
|
Therapeutic Interventions
Antimicrobial therapy was dynamically adjusted (Table 1). (1) Legionella-targeted therapy [(Moxifloxacin (400mg IV q24h) + azithromycin (500mg IV q24h)] initiated on Day 1. (2) Immunomodulation: Methylprednisolone (40mg IV q24h) started on Day 2, ends on Day 7. (3) Antifungal therapy: Fluconazole (800mg loading, then 400mg q24h) on Day 6; switched to amphotericin B lipid complex (5mg/kg/day) on Day 11 due to persistent fever and rising β-D-glucan (↑832 pg/mL). (4) Broad-spectrum coverage: Imipenem-cilastatin (1000mg q12h) maintained until Day 10; sulbactam/cefoperazone added on Day 11 for suspected gram-negative coinfection. (5) Biomarker-guided response assessment: PCT declined from 42.55 → 9.23 ng/mL by Day 7 (bacterial control). CRP spiked to 256.2 mg/mL on Day 7 (fungal breakthrough), declining to 58.8 mg/mL after amphotericin B (Figure 3). (6) Supportive care: Hemodialysis (3×/week) for fluid/electrolyte management. Non-invasive ventilation (FiO2 50%, PEEP 8 cmH2O).
 |
Table 1 Key Diagnostic and Therapeutic Timeline
|
Outcome and Follow-up
Day 20: CT showed >70% resolution of consolidations (Figure 1C).
Day 23: Discharged with oral levofloxacin (750mg q24h) and posaconazole (300mg q24h).
1-month follow-up: PCT 0.3 ng/mL, CRP 6 mg/L. Renal function stabilized (creatinine 201 μmol/L).
Diagnostic Validation and Quality Control
Pre-analytical: Respiratory tract samples processed within 1 hour (cold chain maintained).
Analytical: dPCR inhibition resolved by protocolized dilution (validated with spike-in controls). mNGS human DNA depletion efficiency: 98.7%.
Post-analytical: Legionella results communicated to clinicians within 4 hours of validation. Multidisciplinary review of discordant results (microbiologist, intensivist, pharmacist).
Discussion
Multi-Platform Molecular Diagnostics
The “stealth” nature of L. pneumophila – characterized by fastidious growth, nonspecific symptoms, and high mortality in immunocompromised hosts (up to 80% if untreated) – demands rapid diagnostic innovation.11 This case demonstrates a tripartite molecular strategy that overcomes traditional barriers: Isothermal amplification provided critical first-line detection within 12h (vs 3–7 days for culture), triggering life-saving macrolide/fluoroquinolone therapy.12 The initial positivity (Figure 2A) was pivotal given the patient’s rapid respiratory deterioration. dPCR’s dilution-reflex protocol resolved false negatives caused by nucleic acid inhibition (undiluted: negative; 10× dilution: 4,455 copies/mL). This phenomenon, attributed to polymerase competition at high DNA concentrations,13 underscores the necessity of standardized validation workflows for quantitative molecular tools. mNGS independently confirmed Legionella dominance (384,661 reads) while revealing clinically significant C. glabrata coinfection (3,473 reads + elevated β-D-glucan), enabling comprehensive antimicrobial coverage.14 This represents the first validated “Screen-Quantify-Expand” algorithm for respiratory pathogens, reducing diagnostic time by >72h versus culture-dependent pathways.
A multi-center epidemiological study of severe community-acquired pneumonia (SCAP) has demonstrated that molecular diagnostics (including PCR and mNGS) demonstrate superior performance in rapidly detecting atypical pathogens. While culture and antigen tests are more accessible, the combined pathogen testing upon hospital admission for SCAP patients is recommended, as the clinical benefit and potential mortality reduction from appropriate targeted therapy outweigh the initial cost.15 Although nucleic acid amplification techniques have been widely applied in pathogen detection with the advancement of molecular methods, promoting the adoption of such integrated molecular diagnostic approaches requires practical considerations at three levels at least, beyond cost: 1) Defined diagnostic stewardship: Establishing clear clinical criteria for test deployment (eg, in severe pneumonia or immunocompromised hosts unresponsive to initial therapy) is essential to ensure appropriate use and resource allocation. 2) Integrated interpretation frameworks: Implementing multidisciplinary team reviews (involving intensivists, clinical microbiologists, and pharmacists) is critical for accurately interpreting complex, multi-platform results and translating them into timely, targeted therapeutic actions. 3) Standardized operational pathways: Developing standardized protocols encompassing pre-analytics (sample processing), analytics (eg, inhibition checks via dilution), and post-analytics (structured reporting) is fundamental to ensuring reliability and reproducibility across different institutions.
Biomarker-Driven Antimicrobial Stewardship
Immunocompromised hosts with pneumonia exhibit 34–68% polymicrobial infection rates,2 yet differentiating colonization from invasion remains challenging. Our case illustrates how serial biomarker profiling optimizes stewardship: PCT- guided bacterial de-escalation: The rapid decline (42.55 → 8.2 ng/mL by Day 7) confirmed Legionella treatment efficacy (Figure 3), allowing cessation of empiric carbapenems. This aligns with PCT’s high negative predictive value (94%) for bacterial clearance.8 CRP biphasic response as a therapeutic compass: Initial decline was seen on Day 5, CRP dropped from 228.2 to 96.8 mg/L after initiating moxifloxacin/azithromycin, suggesting partial inflammatory control. Secondary surge was seen by Day 6, CRP rebounded to 256.2 mg/L despite antifungal escalation (fluconazole → amphotericin B) and imipenem doubling on Day 6. This paradoxical rise reflects two intertwined factors: (1) Legionella’s intrinsic slow response: Even appropriate therapy requires 48–72 hours for significant biomarker improvement due to intracellular persistence.16 (2) Antifungal lag phase: Amphotericin B’s maximal effect against C. glabrata manifests after 48–96 hours.17
This biphasic CRP pattern underscores that in immunocompromised hosts, biomarker trends must be interpreted within pathogen-specific response timelines. Early immunomodulation with methylprednisolone may have mitigated systemic inflammation in this critically ill patient with multiorgan dysfunction. Premature regimen abandonment based on transient CRP rise could jeopardize outcomes. Dual-trending PCT (bacterial burden) and CRP (inflammatory activity) thus creates a nuanced “infection barometer” – a strategy critical for mixed-infection management.18
Antifungal Management in Renal-Impaired Hosts: Balancing Efficacy and Toxicity
The emergence of C. glabrata in this renal failure patient posed unique challenges: Fluconazole failure was anticipated (inherent resistance in 15–20% of C. glabrata19) yet initiated empirically due to renal safety concerns. Amphotericin B optimization: Lipid formulation dosing (5 mg/kg/day) required therapeutic drug monitoring (target trough 1–2 μg/mL) to mitigate nephrotoxicity, with parallel hemodialysis mitigating electrolyte disturbances.20 Biomarker-driven duration: β-D-glucan decline from 832 to normal guided 14-day amphotericin B course, avoiding prolonged exposure. Contrast with typical legionellosis: While pure Legionella pneumonia rarely requires >10–14 days therapy,21 coinfection extended treatment to 23 days, highlighting the impact of comorbidities on antimicrobial planning.
Diagnostic Stewardship: Laboratory-Clinician Synergy
This case exemplifies how proactive laboratory engagement optimizes clinical outcomes through integrated pre-analytical, analytical, and post-analytical interventions: Pre-analytical, BALF processing within 1 hour under validated cold-chain conditions (4°C) preserved nucleic acid integrity. During analysis, protocolized dilution resolved dPCR inhibition while 98.7% human mNGS human DNA depletion enhanced pathogen detection. Post-analytically, Legionella positivity was communicated to the ICU within 4 hours, and fungal reads from mNGS triggered consequent β-D-glucan monitoring.
Limitations and Translational Perspectives
Despite its success, this approach faces hurdles: Cost-effectiveness remains a concern: mNGS and dPCR add approximately $800 per test compared to $50 for conventional culture.22 However, the potential reduction in ICU stay may partially offset these expenses.23 Technical barriers also exist: dPCR availability is still limited, while isothermal amplification assays cover only a narrow spectrum of respiratory pathogens. Future directions should focus on: (1) Developing point-of-care platforms for rapid quantification. (2) Leveraging host-response transcriptomics to differentiate colonization from invasion,24 and (3) Integrating AI with biomarker trends to enable automated clinical alerts.25
Conclusion
This case redefines diagnostic paradigms for severe pneumonia in immunocompromised hosts. The synergistic use of isothermal amplification, dPCR, and mNGS enabled rapid, accurate identification of L. pneumophila and C. glabrata, overcoming limitations of single platforms. Dynamic PCT/CRP monitoring optimized antimicrobial stewardship, while laboratory-clinical communication ensured timely intervention. While this integrated model offers a promising template for managing complex infections, its broader adoption faces barriers including cost, technical complexity, and the need for standardized protocols and interdisciplinary collaboration. Future efforts should focus on developing cost-effective point-of-care platforms, establishing clear diagnostic pathways for high-risk patients, and validating their impact on patient outcomes through multi-center studies. As molecular diagnostics evolve, this approach underscores that precision medicine in critical care begins with precision diagnostics, though its implementation requires careful consideration of practical and economic factors alongside clinical benefit.
Ethical Approval
The study was approved by the Research Ethics Committee of Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University (KY2023-405-02). Institutional approval was also required and obtained for the publication of the case details. All procedures performed were in accordance with the ethical standards of the institutional research committee and with the principles outlined in the Declaration of Helsinki and its amendments. The strains involved in the study were residual clinical isolates, without animal experiments and animal ethical requirements.
Consent Statement
Written informed consent was obtained from the patient for academic publication, including any accompanying images and case details.
Acknowledgments
The study was supported by various colleagues from the hospital’s Department of Clinical Laboratory.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the National Natural Science Foundation of China (Grant No. 82302571); Basic and Applied Basic Research Foundation of Guangdong (2024A1515011037); Medical Science and Technology Research Foundation of Guangdong (B2025152).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Nair GB, Niederman MS. Updates on community acquired pneumonia management in the ICU. Pharmacol Ther. 2021;217:107663. doi:10.1016/j.pharmthera.2020.107663
2. Azoulay E, Russell L, Van de Louw A, et al. Diagnosis of severe respiratory infections in immunocompromised patients. Intensive Care Med. 2020;46(2):298–314. doi:10.1007/s00134-019-05906-5
3. Mondino S, Schmidt S, Rolando M, et al. Legionnaires’ disease: state of the art knowledge of pathogenesis mechanisms of legionella. Annu Rev Pathol. 2020;15(1):439–466. doi:10.1146/annurev-pathmechdis-012419-032742
4. Cunha BA, Burillo A, Bouza E. Legionnaires’ disease. Lancet. 2016;387(10016):376–385. doi:10.1016/S0140-6736(15)60078-2
5. Chahin A, Opal SM. Severe pneumonia caused by legionella pneumophila: differential diagnosis and therapeutic considerations. Infect Dis Clin North Am. 2017;31(1):111–121. doi:10.1016/j.idc.2016.10.009
6. Romanov KA, O’Connor TJ. Legionella pneumophila, a Rosetta stone to understanding bacterial pathogenesis. J Bacteriol. 2024;206(12):e0032424. doi:10.1128/jb.00324-24
7. Viasus D, Gaia V, Manzur-Barbur C, Carratalà J. Legionnaires’ disease: update on diagnosis and treatment. Infect Dis Ther. 2022;11(3):973–986. doi:10.1007/s40121-022-00635-7
8. Yue R, Wu X, Li T, et al. Early detection of legionella pneumophila and aspergillus by mNGS in a critically Ill patient with legionella pneumonia after extracorporeal membrane oxygenation treatment: case report and literature review. Front Med Lausanne. 2021;8:686512. doi:10.3389/fmed.2021.686512
9. Wu J, Tang B, Qiu Y, et al. Clinical validation of a multiplex droplet digital PCR for diagnosing suspected bloodstream infections in ICU practice: a promising diagnostic tool. Crit Care. 2022;26(1):243. doi:10.1186/s13054-022-04116-8
10. Keikha M. LAMP method as one of the best candidates for replacing with PCR method. Malays J Med Sci. 2018;25(1):121–123. doi:10.21315/mjms2018.25.1.15
11. Kümpers P, Tiede A, Kirschner P, et al. Legionnaires’ disease in immunocompromised patients: a case report of Legionella longbeachae pneumonia and review of the literature. J Med Microbiol. 2008;57(Pt 3):384–387. doi:10.1099/jmm.0.47556-0
12. Fraser DW, Tsai TR, Orenstein W, et al. Legionnaires’ disease: description of an epidemic of pneumonia. N Engl J Med. 1977;297(22):1189–1197. doi:10.1056/NEJM197712012972201
13. Dong L, Meng Y, Sui Z, et al. Comparison of four digital PCR platforms for accurate quantification of DNA copy number of a certified plasmid DNA reference material. Sci Rep. 2015;5(1):13174. doi:10.1038/srep13174
14. Azoulay E, Mokart D, Kouatchet A, et al. Acute respiratory failure in immunocompromised adults. Lancet Respir Med. 2019;7(2):173–186. doi:10.1016/S2213-2600(18)30345-X
15. Qu J, Zhang J, Chen Y, et al. Aetiology of severe community acquired pneumonia in adults identified by combined detection methods: a multi-centre prospective study in China. Emerg Microbes Infect. 2022;11(1):556–566. doi:10.1080/22221751.2022.2035194
16. Price C, Jones S, Mihelcic M, et al. Paradoxical pro-inflammatory responses by human macrophages to an amoebae host-adapted legionella effector. Cell Host Microbe. 2020;27(4):571–584.e7. doi:10.1016/j.chom.2020.03.003
17. Puumala E, Fallah S, Robbins N, Cowen LE. Advancements and challenges in antifungal therapeutic development. Clin Microbiol Rev. 2024;37(1):e0014223. doi:10.1128/cmr.00142-23
18. Ohta R, Hattori S, Inoue K, Sano C. Difficulty in diagnosing and treating a prostate abscess with bacterial and fungal coinfection in an immunocompromised patient. Cureus. 2022;14(1):e21774. doi:10.7759/cureus.21774
19. Katsipoulaki M, Stappers MHT, Malavia-Jones D, Brunke S, Hube B, Gow NAR. Candida albicans and Candida glabrata: global priority pathogens. Microbiol Mol Biol Rev. 2024;88(2):e0002123. doi:10.1128/mmbr.00021-23
20. Hamill RJ. Amphotericin B formulations: a comparative review of efficacy and toxicity. Drugs. 2013;73(9):919–934. doi:10.1007/s40265-013-0069-4
21. Heath CH, Grove DI, Looke DF. Delay in appropriate therapy ofLegionella pneumonia associated with increased mortality. Eur J Clin Microbiol Infect Dis. 1996;15(4):286–290. doi:10.1007/BF01695659
22. Simner PJ, Miller S, Carroll KC. Understanding the promises and hurdles of metagenomic next-generation sequencing as a diagnostic tool for infectious diseases. Clin Infect Dis. 2018;66(5):778–788. doi:10.1093/cid/cix881
23. Li S, Tong J, Li H, et al. L. pneumophila infection diagnosed by tNGS in a lady with lymphadenopathy. Infect Drug Resist. 2023;16:4435–4442. doi:10.2147/IDR.S417495
24. Vormittag S, Hüsler D, Haneburger I, et al. Legionella – and host-driven lipid flux at LCV-ER membrane contact sites promotes vacuole remodeling. EMBO Rep. 2023;24(3):e56007. doi:10.15252/embr.202256007
25. Tang S, Shepard S, Clark R, et al. Guiding clostridioides difficile infection prevention efforts in a hospital setting with AI. JAMA Network Open. 2025;8(6):e2515213. doi:10.1001/jamanetworkopen.2025.15213