Comet C/2025 A6 Lemmon on Oct. 11, 2025, as imaged by Gianluca Masi at The Virtual Telescope Project (www.virtualtelescope.eu).
Gianluca Masi at The Virtual Telescope Project (www.virtualtelescope.eu). Used with permission.
Check my feed every day…

Comet C/2025 A6 Lemmon on Oct. 11, 2025, as imaged by Gianluca Masi at The Virtual Telescope Project (www.virtualtelescope.eu).
Gianluca Masi at The Virtual Telescope Project (www.virtualtelescope.eu). Used with permission.
Check my feed every day…
The Phase 3 FLAURA2 trial (NCT04035486) continues to strengthen the role of combination therapy in the first-line management of EGFR-mutated (EGFRm) advanced non–small cell lung cancer (NSCLC). At ESMO 2025, investigators reported the final overall survival (OS) analysis, showing that osimertinib (osi) plus platinum–pemetrexed chemotherapy (CTx) achieved a statistically significant and clinically meaningful OS improvement compared with osimertinib monotherapy.
This milestone confirms the combination as a first-line standard of care in EGFRm NSCLC, offering durable efficacy across key subgroups, including those with traditionally poor prognostic features such as CNS metastases, L858R mutations, plasma-detectable EGFRm, and altered TP53.
The FLAURA2 trial enrolled 557 patients with EGFRm advanced NSCLC, who were randomized 1:1 to receive osimertinib plus chemotherapy (n=279) or osimertinib alone (n=278). The chemotherapy regimen consisted of platinum–pemetrexed, administered concurrently with osimertinib.
Baseline CNS imaging (CT or MRI) was mandatory to identify central nervous system metastases. EGFR mutation subtypes (Ex19del or L858R) were confirmed through central or locally approved assays. Plasma EGFR mutation detection was evaluated via droplet digital PCR (Biodesix), while TP53 mutation status was determined using FoundationOne CDx.
OS outcomes were analyzed using an unstratified Cox proportional hazards model, with subgroup analyses conducted based on baseline prognostic factors.
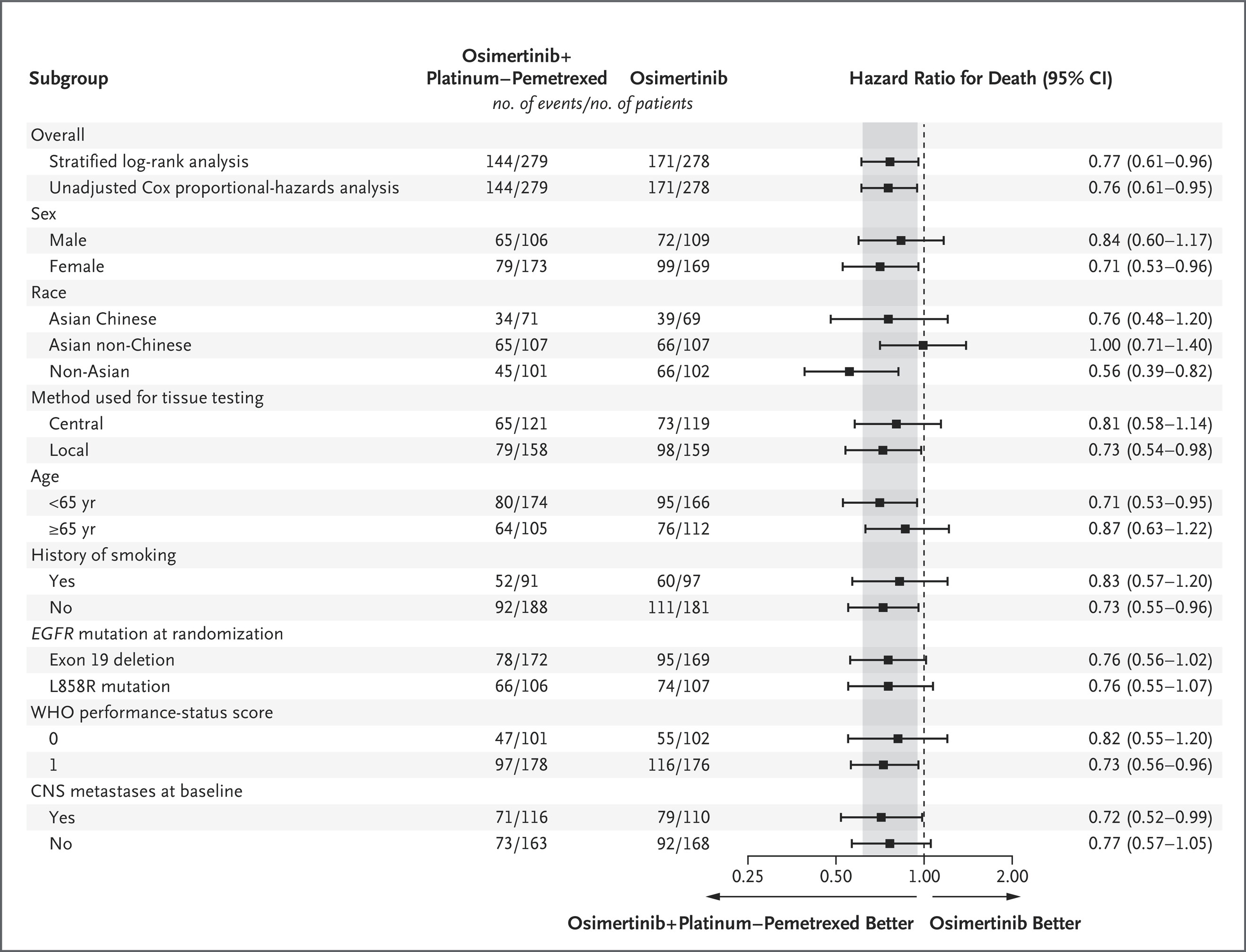
A total of 557 patients were included: 279 in the osimertinib + CTx arm and 278 in the osimertinib monotherapy arm. The overall hazard ratio (HR) for OS was 0.77 (95% CI 0.61–0.96; p=0.02), corresponding to a 23% reduction in risk of death with the combination regimen.
In patients with baseline CNS metastases, median OS reached 40.9 months (95% CI 35.2–46.6) with osimertinib + CTx versus 29.7 months (95% CI 25.6–35.8) with monotherapy (HR 0.72; 95% CI 0.52–0.99).
Both EGFRm subgroups derived benefit.
Patients with detectable plasma EGFRm achieved median OS 38.4 vs 32.5 months (HR 0.79; 95% CI 0.60–1.03), while those with undetectable mutations had not reached median OS in either arm.
Among patients with altered TP53, OS improved to 51.1 months vs 43.1 months (HR 0.71; 95% CI 0.40–1.27), showing consistent benefit across molecular profiles.
No new safety signals were reported, confirming that the addition of chemotherapy did not compromise the established tolerability of osimertinib.
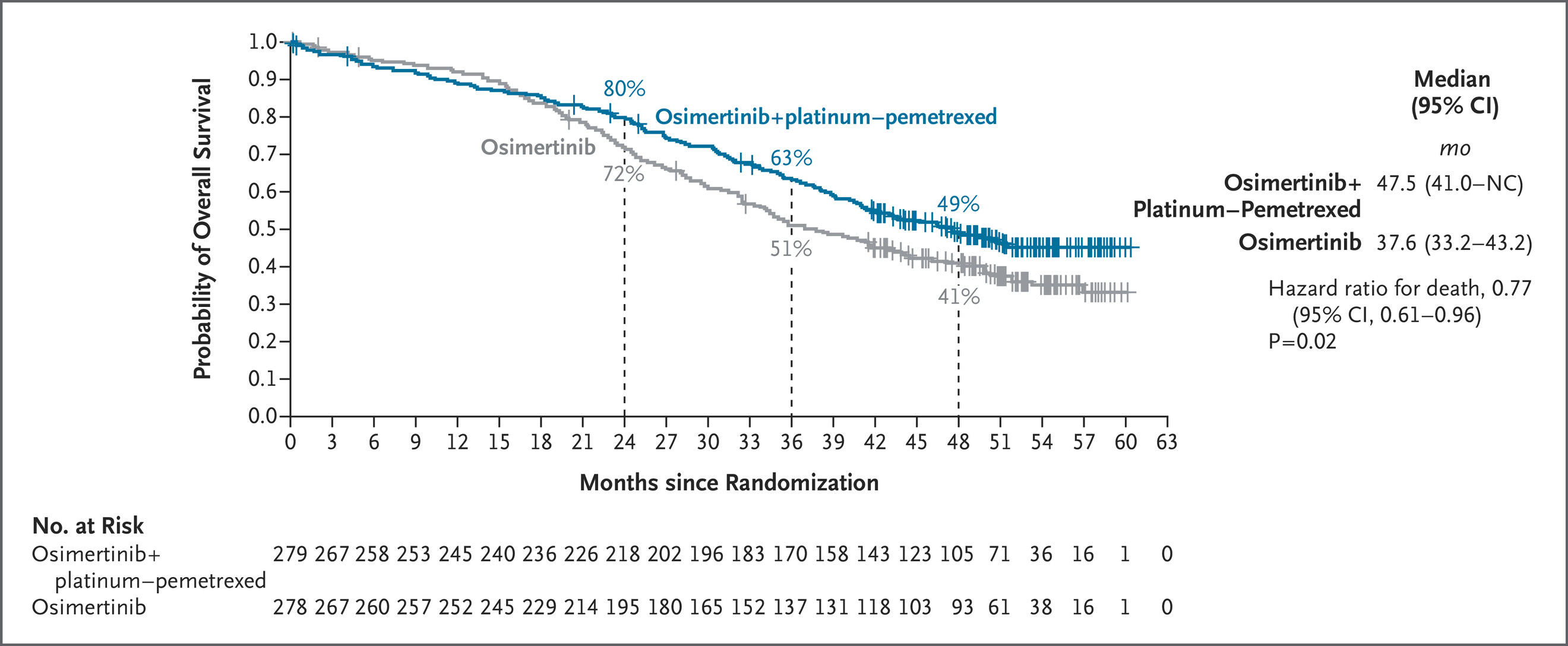
The survival improvement observed with osimertinib plus chemotherapy extended across every prognostic subgroup examined. The HRs for OS within each category closely mirrored those of the overall intent-to-treat (ITT) population, highlighting the robustness and reproducibility of the benefit.
Particularly noteworthy were the gains among patients with CNS metastases and L858R mutation, two subsets traditionally associated with poorer prognosis. These data underline the capacity of the combination regimen to overcome key resistance mechanisms and delay disease progression.
The long-term follow-up from the FLAURA2 trial at ESMO 2025 provides the most comprehensive survival dataset to date for EGFR-mutated NSCLC treated with first-line osimertinib plus chemotherapy. With several subgroups not yet reaching median OS, the sustained separation of survival curves indicates a persistent and cumulative treatment effect extending well beyond the chemotherapy phase.
Investigators emphasized that the survival curves for osimertinib + CTx began to diverge early—within the first year of treatment—and remained separated throughout follow-up, suggesting that early dual blockade of EGFR signaling and microenvironmental suppression via chemotherapy offers durable control of micrometastatic disease.
The analysis also highlights that median OS was not reached in multiple subgroups, demonstrating an ongoing trend toward improved long-term outcomes. The consistency of benefit across genomic and clinical subgroups—including those with TP53 alterations or detectable circulating tumor DNA—supports the biological rationale that concurrent chemotherapy may help prevent the emergence of resistant clones.
Methodologically, the trial’s unstratified Cox model ensured unbiased subgroup comparisons and confirmed that the treatment effect was independent of baseline risk characteristics. Furthermore, despite crossover and subsequent therapies available post-progression, the OS advantage with osimertinib plus chemotherapy persisted, reinforcing the value of front-line combination therapy over sequential monotherapy strategies.
No late-emerging toxicities or cumulative safety concerns were identified during long-term follow-up, strengthening the safety profile of the regimen. Together, these findings establish osimertinib plus chemotherapy as a durable, well-tolerated, and biologically rational first-line standard of care for patients with EGFR-mutated advanced NSCLC.
Read Full Abstract on ESMO Congress 2025 Website
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
AOL is part of the Yahoo family of brands.

PATIENT and public involvement and engagement (PPIE) is increasingly recognised as a cornerstone of ethical medical research, particularly in allergic diseases. The 2024 Revision of the Declaration of Helsinki emphasises that research must…

Published on: Oct 19, 2025 01:30 pm IST

First Period
It was the visitors who came out of the traps quickest and made Jackson Whistle work. Vlastimil Dostalek rattled the crossbar before Whistle made a good blocker save from Jaka Sturm. Momentum would swing back towards the…

Delete all these texts.
getty
Text attacks on Android and iPhone owners in America, Europe and elsewhere are totally out of control. This billion-dollar industry now defrauds millions of smartphone owners. The malicious technologies that execute…
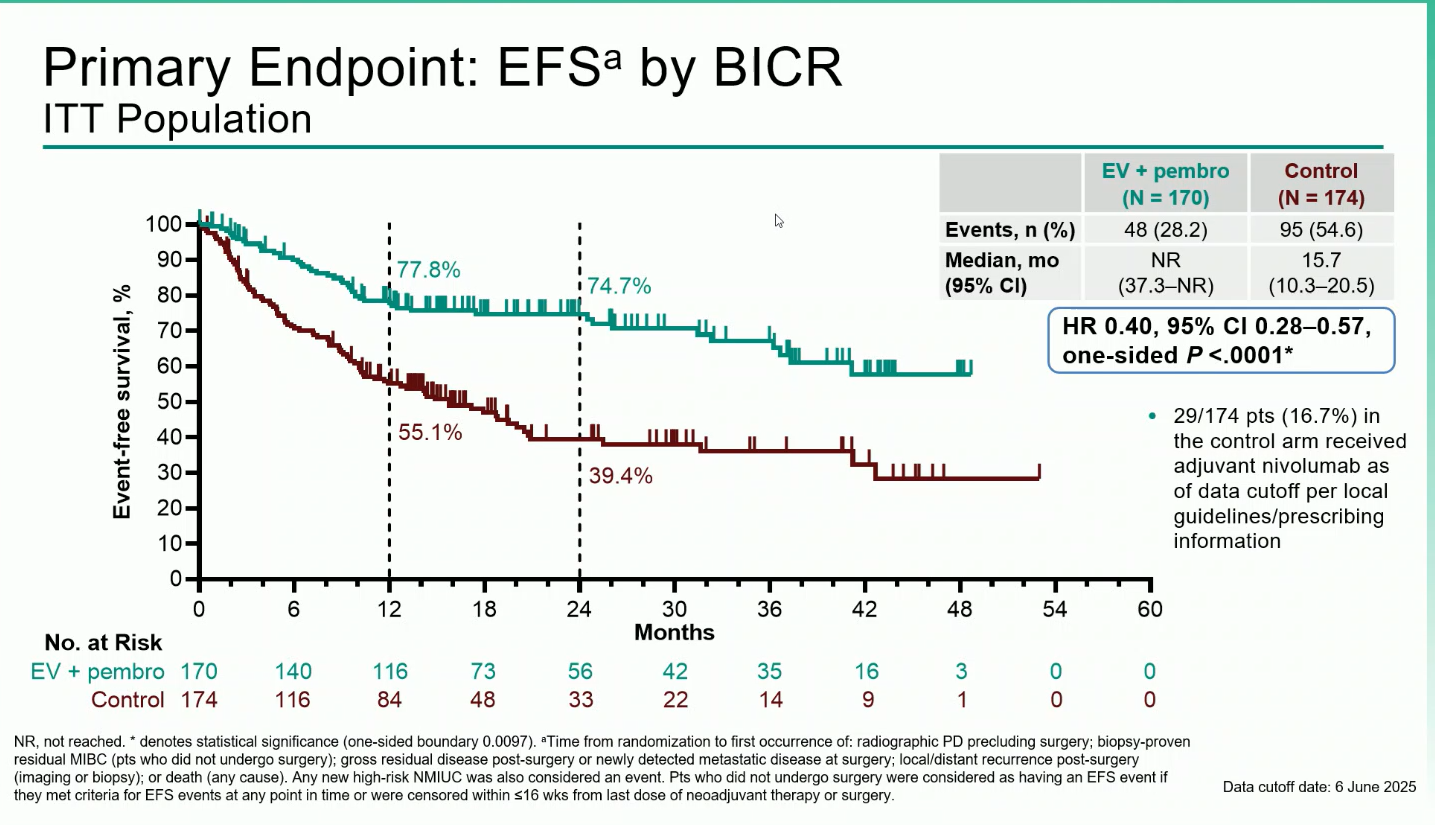
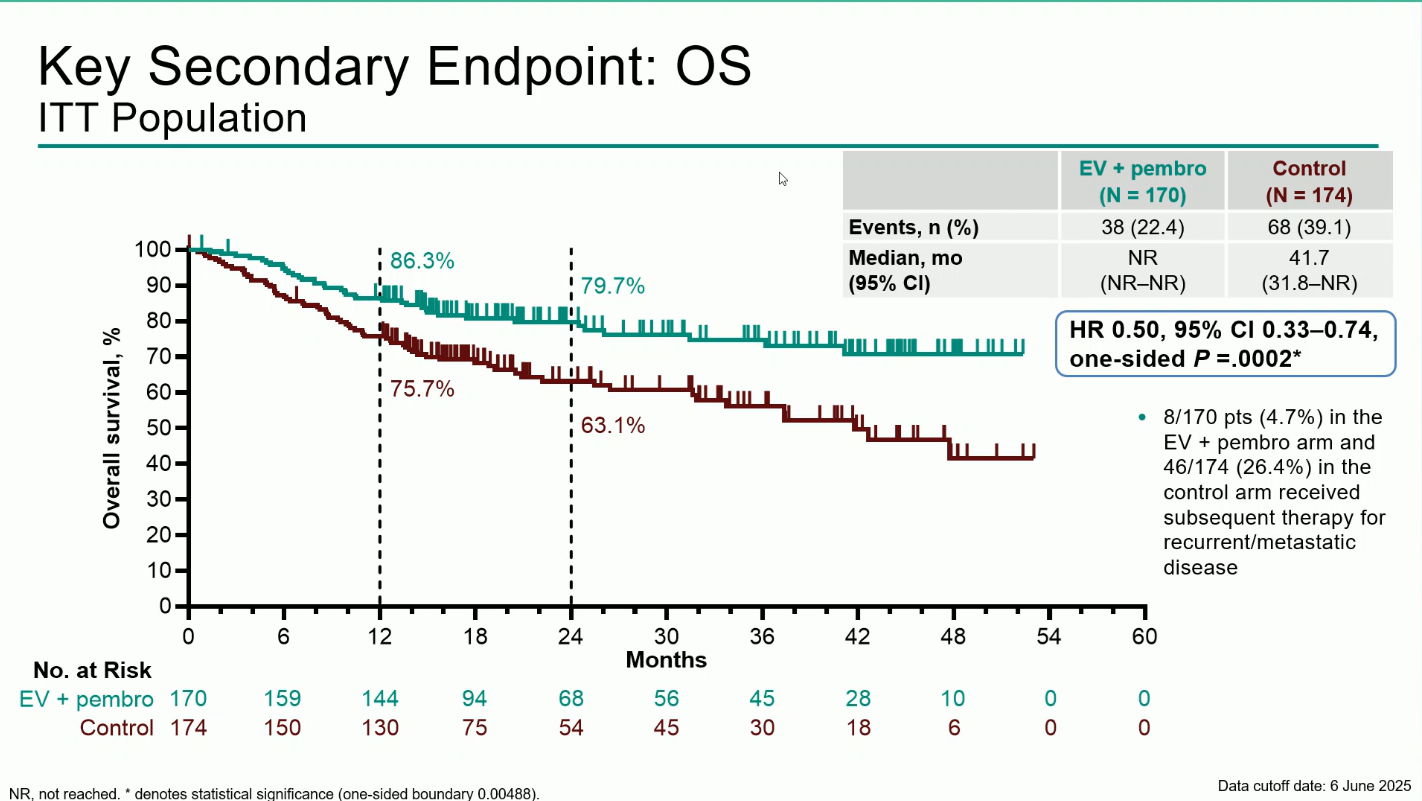
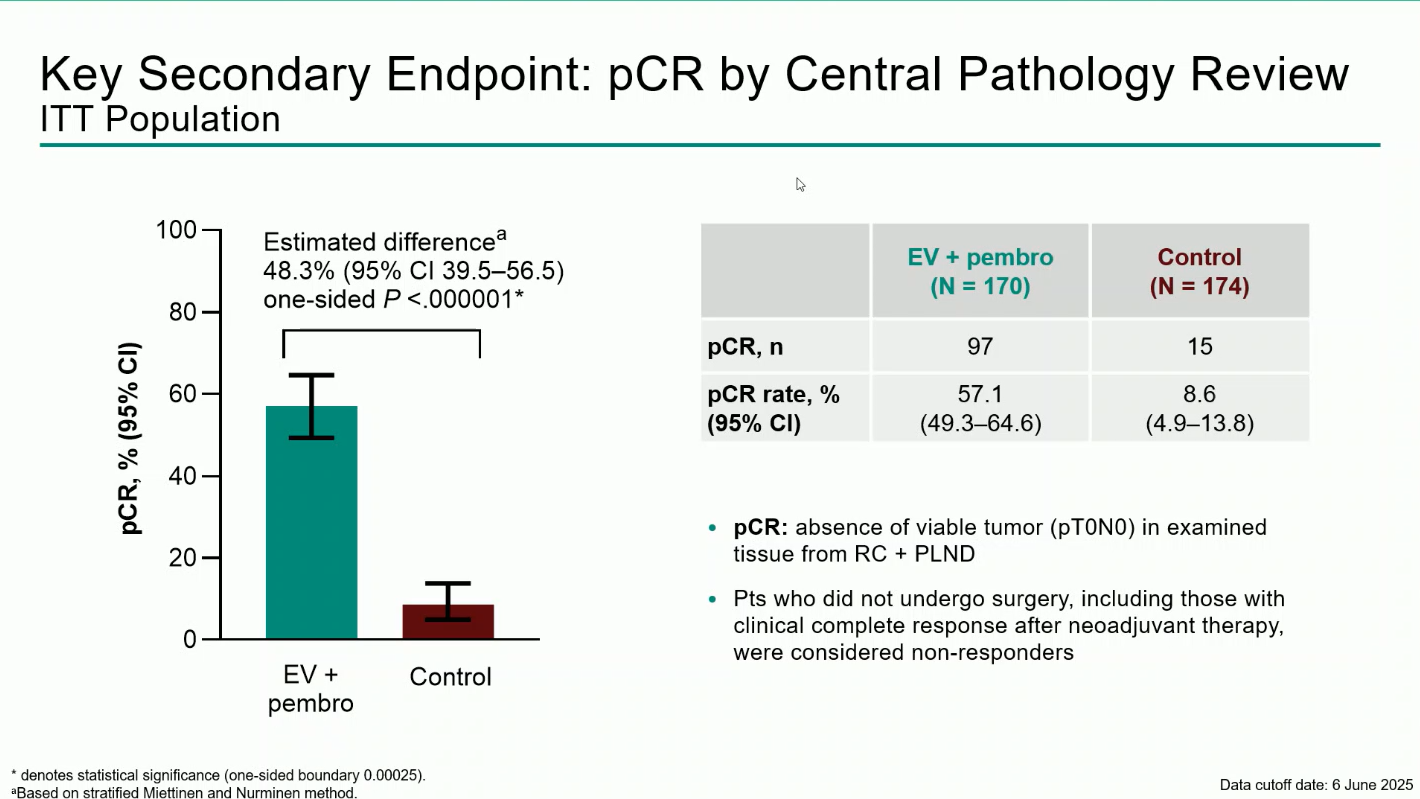
KEYNOTE-905/EV-303 (NCT03924895), a phase 3, open-label, randomized trial, evaluated perioperative enfortumab vedotin (EV) plus pembrolizumab (pembro) compared with surgery alone in patients with muscle-invasive bladder cancer (MIBC) who were ineligible for or declined cisplatin-based chemotherapy.
Presented by Prof. Christof Vulsteke at the ESMO Congress 2025, the study demonstrated that adding EV + pembro to radical cystectomy with pelvic lymph node dissection resulted in significant improvements in event-free survival (EFS), overall survival (OS), and pathologic complete response (pCR). These findings mark a major advance for cisplatin-ineligible MIBC, establishing a potential new perioperative standard of care.
Radical cystectomy with pelvic lymph node dissection (RC + PLND) remains the standard of care for patients with muscle-invasive bladder cancer. However, nearly half of these patients are ineligible for cisplatin-based chemotherapy due to renal dysfunction, frailty, or comorbidities, leaving a substantial population without effective perioperative options.
Previous studies have shown limited benefit from surgery alone in this setting, underscoring the unmet need for alternative strategies. Enfortumab vedotin, an antibody–drug conjugate targeting Nectin-4, combined with pembrolizumab, has demonstrated potent antitumor activity and a favorable safety profile in metastatic urothelial cancer, providing a strong rationale for evaluation in the perioperative context.
KEYNOTE-905/EV-303 is a randomized, open-label, phase 3 trial that enrolled adults with MIBC (T2–T4aN0M0 or T1–T4aN1M0) who were cisplatin-ineligible per Galsky criteria or declined cisplatin.
Participants were randomized 1:1 to receive:
The primary endpoint was event-free survival (EFS) by blinded independent central review (BICR).Key secondary endpoints included overall survival (OS), pathologic complete response (pCR), and safety.
A total of 344 participants were randomized between December 2020 and June 2024 (170 to EV + pembro; 174 to control). Over 80% were cisplatin-ineligible, and the median follow-up was 25.6 months (range 11.8–53.7).The combination regimen produced statistically significant and clinically meaningful improvements across all efficacy endpoints:
Treatment-emergent adverse events (TEAEs) occurred in nearly all patients (100% in EV + pembro vs 64.8% in control). Grade ≥3 events were reported in 71.3% and 45.9%, respectively. The most frequent grade ≥3 adverse events of special interest were severe skin reactions (11.4%) related to pembrolizumab and cutaneous toxicity (10.8%) associated with enfortumab vedotin.
Despite the high incidence of AEs, the safety profile remained manageable and consistent with prior studies, and no new safety signals were identified.
The KEYNOTE-905/EV-303 trial demonstrated that adding perioperative enfortumab vedotin plus pembrolizumab to standard surgery significantly improved event-free survival, overall survival, and pathologic complete response rates in patients with cisplatin-ineligible MIBC.
These findings establish EV + pembrolizumab as the first perioperative regimen to improve outcomes versus RC + PLND alone in this population, offering a potential new standard of care.
You can read the full abstract here.

KARACHI: Experienced wicketkeeper-batter Mohammad Rizwan’s captaincy in the 50-overs format could be on the line when a joint meeting of the national selection committee and advisory board of the Pakistan Cricket Board (PCB) is held on Monday in…