New drugs that target ‘zombie’ tuberculosis (TB) cells are now a step closer, thanks to a new study led by the University of Surrey, published in Scientific Reports.
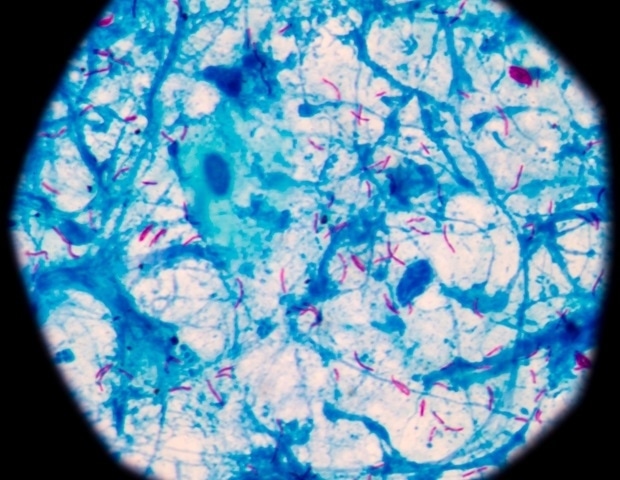
Many dangerous pathogens, including the bacteria that cause TB, are capable of generating dormant, drug-tolerant cells, often described as ‘zombies’. These persister cells can survive intense antibiotic treatments by essentially playing dead. Once the drugs are gone, they ‘wake up’ and can trigger recurring, and often deadly, infections. Eliminating these zombie-like cells currently requires months of multi-drug therapy, and even then, treatment often fails, fueling relapse and the rise of antimicrobial resistance (AMR).
In the study, the Surrey team exposed a vast library of over 500,000 genetically modified TB bacteria to two commonly used antibiotics – rifampicin and streptomycin. The exposure was extended long enough that the remaining survivors were primarily persisters. By analyzing the survivors, the researchers pinpointed genes whose disruption significantly reduced the number of surviving zombie cells.
These critical genes were found to perform various roles: some weakened the protective bacterial cell wall, others activated a form of bacterial self-destruction, and still others disrupted the cell’s metabolic balance. Each of these pathways offers a potential strategy for designing new drugs that could wipe out persister cells more rapidly and effectively.
The next phase of research will focus on developing novel therapeutics that mimic these gene functions, paving the way for shorter, more successful TB treatments and a powerful new weapon in the global fight against AMR.
Tuberculosis really is the forgotten pandemic. It killed 1.3 million people last year, mostly from completely drug-sensitive strains. The problem isn’t always resistance – it’s persisters. These are a tiny group of phenotypically drug-resistant bacteria that survive antibiotic treatment and can go on to cause treatment failure.
What we found is that persister survival depends on the antibiotic used. The mechanisms aren’t shared as previously thought; they’re drug-specific. That changes how we think about targeting persisters and could shape how future TB treatments are designed.”
Dr. Suzie Hingley-Wilson, co-corresponding author of the study and Senior Lecturer in Bacteriology at the University of Surrey
Mutations in some of the genes identified in the study have been found in TB strains from patients who do not respond to treatment. This overlap suggests that the mechanisms observed in the lab reflect what is happening in real infections and may help explain why some patients relapse even when the bacteria are not resistant to the antibiotics.
Professor Johnjoe McFadden, study lead from the University of Surrey, said:
“The mechanisms involved in persistence are probably the biggest mysteries in microbiology. Their solution could revolutionize treatment for some of the most challenging diseases to treat, such as tuberculosis (TB). This groundbreaking research could lead to new drugs that target persisters, shortening treatment regimens and reducing both treatment costs and the burden of antimicrobial resistance (AMR).”
The study was supported by the Medical Research Council and the Biotechnology and Biological Sciences Research Council.
Source:
Journal reference:
Toloza, J. E. H., et al. (2025). The identification Mycobacterium tuberculosis genes that modulate long term survival in the presence of rifampicin and streptomycin. Scientific Reports. doi.org/10.1038/s41598-025-04038-9.