Living organisms quietly emit light. This glow is real, measurable, and tied to life itself. Researchers at the University of Calgary and the National Research Council of Canada have now shown that this ultraweak light fades sharply after death,…
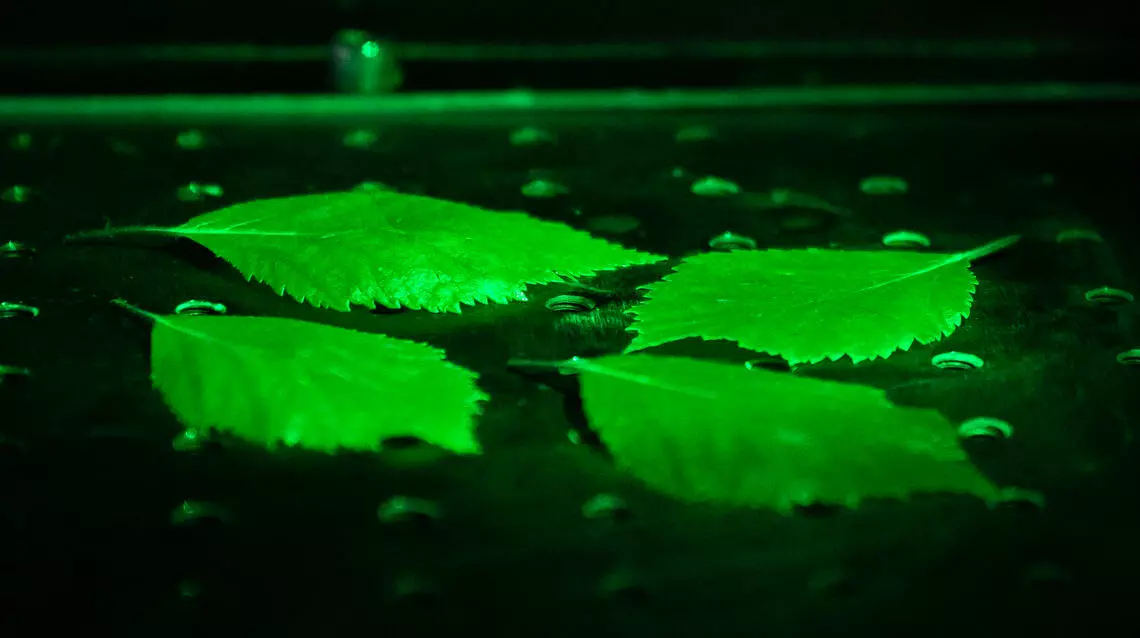
Living organisms quietly emit light. This glow is real, measurable, and tied to life itself. Researchers at the University of Calgary and the National Research Council of Canada have now shown that this ultraweak light fades sharply after death,…