Golin R, Godfrey C, Firth J, Lee L, Minior T, Phelps BR, et al. Pepfar’s response to the convergence of the HIV and COVID-19 pandemics in sub-Saharan Africa. J Int AIDS Soc. 2020. https://doi.org/10.1002/jia2.25587.
Google Scholar
Vrazo AC, Golin R, Fernando NB, Killam WP, Sharifi S, Phelps BR, et al. Adapting HIV services for pregnant and breastfeeding women, infants, children, adolescents and families in resource-constrained settings during the COVID-19 pandemic. J Int AIDS Soc. 2020. https://doi.org/10.1002/jia2.25622.
Google Scholar
Mbithi I, Thekkur P, Chakaya JM, Onyango E, Owiti P, Njeri NC, et al. Assessing the real-time impact of COVID-19 on TB and HIV services: the experience and response from selected health facilities in Nairobi, Kenya. Trop Med Infect Dis. 2021;6: 74. https://doi.org/10.3390/tropicalmed6020074.
Google Scholar
Chitungo I, Mhango M, Mbunge E, Dzobo M, Musuka G, Dzinamarira T. Utility of telemedicine in sub-Saharan Africa during the COVID-19 pandemic. A rapid review. Hum Behav Emerg Technol. 2021. https://doi.org/10.1002/hbe2.297.
Google Scholar
Dodoo JE, Al-Samarraie H, Alzahrani AI. Telemedicine use in sub-Saharan Africa: barriers and policy recommendations for Covid-19 and beyond. Int J Med Inform. 2021;151. https://doi.org/10.1016/j.ijmedinf.2021.104467.
Murewanhema G, Mpabuka E, Moyo E, Tungwarara N, Chitungo I, Mataruka K, et al. Accessibility and utilization of antenatal care services in sub-Saharan Africa during the COVID-19 pandemic: a rapid review. Birth. 2023. https://doi.org/10.1111/birt.12719.
Google Scholar
Oyediran KA, Makinde OA, Adelakin O. The role of telemedicine in addressing access to sexual and reproductive health services in sub-saharan africa during the covid-19 pandemic. Afr J Reprod Health. 2020;24. https://doi.org/10.29063/ajrh2020/v24i2s.8.
Lintz J. Adoption of telemedicine during the COVID-19 pandemic: perspectives of primary healthcare providers. Eur J Public Health. 2021. https://doi.org/10.1093/eurpub/ckab165.155.
Google Scholar
Luo J, Tong L, Crotty BH, Somai M, Taylor B, Osinski K, et al. Telemedicine adoption during the COVID-19 pandemic: gaps and inequalities. Appl Clin Inform. 2021. https://doi.org/10.1055/s-0041-1733848.
Google Scholar
Mishra V. Factors affecting the adoption of telemedicine during COVID-19. Indian J Public Health. 2020. https://doi.org/10.4103/ijph.IJPH_480_20.
Google Scholar
Galle A, Semaan A, Huysmans E, Audet C, Asefa A, Delvaux T, et al. A double-edged sword-telemedicine for maternal care during COVID-19: findings from a global mixed-methods study of healthcare providers. BMJ Glob Health. 2021. https://doi.org/10.1136/bmjgh-2020-004575.
Google Scholar
Keith RE, Crosson JC, O’Malley AS, Cromp D, Taylor EF. Using the consolidated framework for implementation research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. 2017;12:1–12. https://doi.org/10.1186/S13012-017-0550-7.
Google Scholar
Mbunge E, Muchemwa B, Batani J. Are we there yet? Unbundling the potential adoption and integration of telemedicine to improve virtual healthcare services in African health systems. Sensors Int. 2022. https://doi.org/10.1016/j.sintl.2021.100152.
Google Scholar
Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians’ adoption of mobile health tools: systematic literature review. JMIR Mhealth Uhealth. 2020. https://doi.org/10.2196/15935.
Google Scholar
Feroz A, Kadir MM, Saleem S. Health systems readiness for adopting mhealth interventions for addressing non-communicable diseases in low- and middle-income countries: a current debate. Glob Health Action. 2018. https://doi.org/10.1080/16549716.2018.1496887.
Google Scholar
Hurt K, Walker RJ, Campbell JA, Egede LE. Mhealth interventions in low and middle-income countries: a systematic review. Glob J Health Sci. 2016;8: https://doi.org/10.5539/gjhs.v8n9p183.
Google Scholar
Peprah P, Abalo EM, Agyemang-Duah W, Budu HI, Appiah-Brempong E, Morgan AK, et al. Lessening barriers to healthcare in rural Ghana: providers and users’ perspectives on the role of mHealth technology. A qualitative exploration. BMC Med Inform Decis Mak. 2020. https://doi.org/10.1186/s12911-020-1040-4.
Google Scholar
Hao WR, Hsu YH, Chen KC, Li HC, Iqbal U, Nguyen PA, et al. Labpush: a pilot study of providing remote clinics with laboratory results via short message service (SMS) in Swaziland, Africa – a qualitative study. Comput Methods Programs Biomed. 2015. https://doi.org/10.1016/j.cmpb.2014.10.005.
Google Scholar
Dharmayat KI, Tran T, Hardy V, Chirambo BG, Thompson MJ, Ide N, et al. Sustainability of ‘mhealth’ interventions in sub-Saharan Africa: A stakeholder analysis of an electronic community case management project in Malawi. Malawi Med J. 2019;31. https://doi.org/10.4314/mmj.v31i3.3.
Njuguna IN, Beima-Sofie K, Mburu CW, Mugo C, Itindi J, Onyango A, et al. Transition to independent care for youth living with HIV: a cluster randomised clinical trial. Lancet HIV. 2022;9: e828–37. https://doi.org/10.1016/S2352-3018(22)00244-2.
Google Scholar
Njuguna IN, Beima-Sofie K, Mburu CW, Mugo C, Neary J, Itindi J, et al. Adolescent transition to adult care for HIV-infected adolescents in Kenya (ATTACH): study protocol for a hybrid effectiveness-implementation cluster randomised trial. BMJ Open. 2020;10: e039972. https://doi.org/10.1136/bmjopen-2020-039972.
Google Scholar
Damschroder L, Hall C, Gillon L, Reardon C, Kelley C, Sparks J, et al. The consolidated framework for implementation research (CFIR): progress to date, tools and resources, and plans for the future. Implement Sci. 2015(S1). https://doi.org/10.1186/1748-5908-10-s1-a12.
Means AR, Kemp CG, Gwayi-Chore MC, Gimbel S, Soi C, Sherr K, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci. 2020. https://doi.org/10.1186/s13012-020-0977-0.
Google Scholar
Creswell J, Plano CV. Designing and Conducting Mixed Methods Research, vol. 1. Third: SAGE Publications Inc; 2017.
Zhang W, Creswell J. The use of mixing procedure of mixed methods in health services research. Med Care. 2013. https://doi.org/10.1097/MLR.0b013e31824642fd.
Google Scholar
Chu PH, Chang YY. John W, Creswell, Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. J Soc Admi Sci. 2017;4.
Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs—principles and practices. Health Serv Res. 2013;48:2134. https://doi.org/10.1111/1475-6773.12117.
Google Scholar
Patridge EF, Bardyn TP. Research electronic data capture (REDCap). J Med Libr Assoc. 2018;106:142.
Google Scholar
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009. https://doi.org/10.1186/1748-5908-4-50.
Google Scholar
Keith RE, Crosson JC, O’Malley AS, Cromp DA, Taylor EF. Using the consolidated framework for implementation research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation. Implement Sci. 2017. https://doi.org/10.1186/s13012-017-0550-7.
Google Scholar
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005. https://doi.org/10.1177/1049732305276687.
Google Scholar
Weiner BJ, Lewis CC, Stanick C, Powell BJ, Dorsey CN, Clary AS, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. 2017;12: 108. https://doi.org/10.1186/s13012-017-0635-3.
Google Scholar
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7. https://doi.org/10.2105/AJPH.89.9.1322.
Google Scholar
Scientific Software Development GmbH. ATLAS.ti: The Qualitative Data Analysis; Research Software. Web 2017.
Rangachari P, Mushiana SS, Herbert K. A scoping review of applications of the consolidated framework for implementation research (CFIR) to telehealth service implementation initiatives. BMC Health Serv Res. 2022. https://doi.org/10.1186/s12913-022-08871-w.
Google Scholar
Tully L, Case L, Arthurs N, Sorensen J, Marcin JP, O’Malley G. Barriers and Facilitators for Implementing Paediatric Telemedicine: Rapid Review of User Perspectives. Front Pediatr. 2021;9. https://doi.org/10.3389/fped.2021.630365.
Williams KM, Kirsh S, Aron D, Au D, Helfrich C, Lambert-Kerzner A, et al. Evaluation of the veterans health administration’s specialty care transformational initiatives to promote patient-centered delivery of specialty care: a mixed-methods approach. Telemed E-Health. 2017. https://doi.org/10.1089/tmj.2016.0166.
Google Scholar
Tagne JF, Burns K, O’Brein T, Chapman W, Cornell P, Huckvale K, et al. Challenges for remote patient monitoring programs in rural and regional areas: a qualitative study. BMC Health Serv Res. 2025;25: 374. https://doi.org/10.1186/s12913-025-12427-z.
Google Scholar
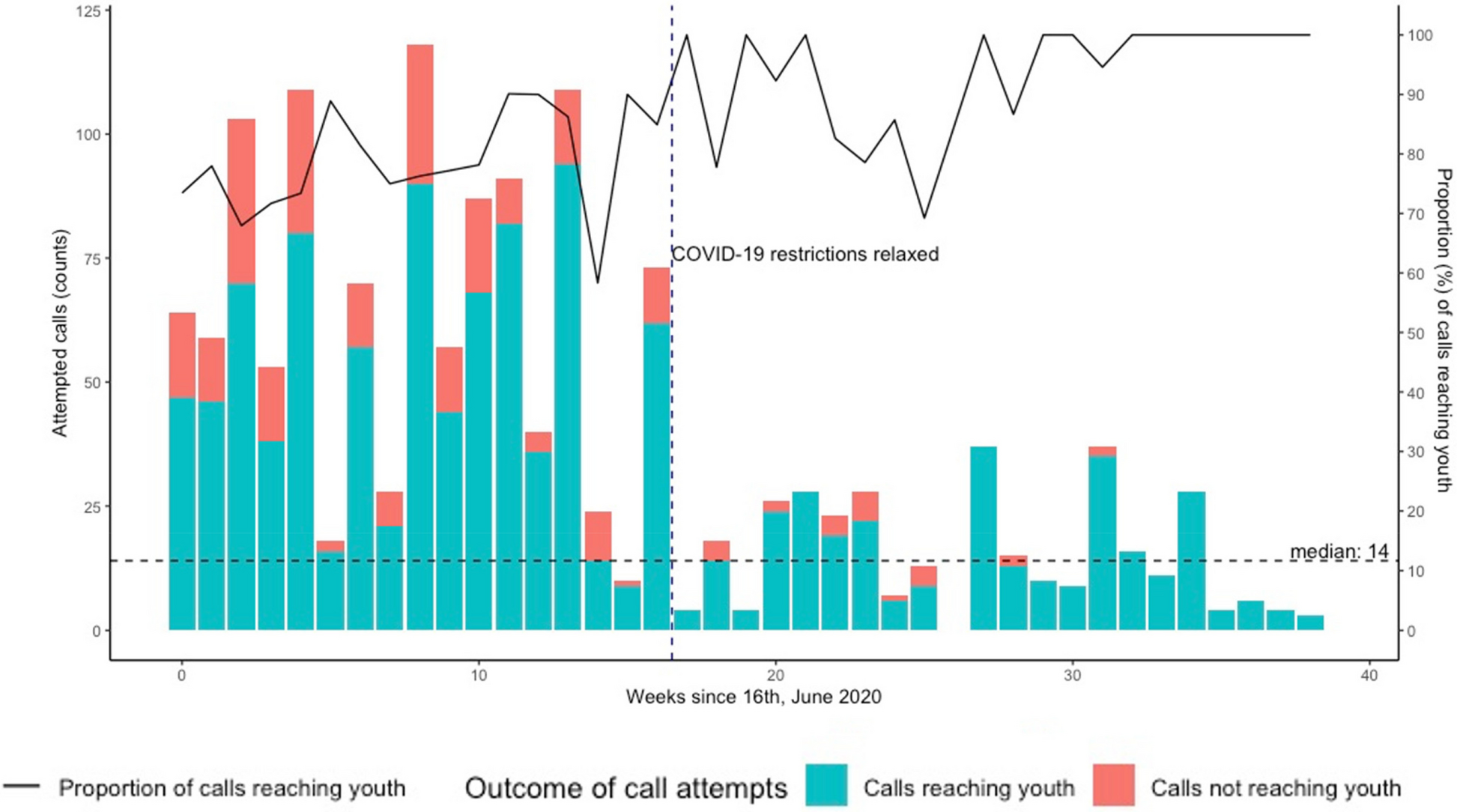
Mangale DI, Onyango A, Mugo C, Mburu C, Chhun N, Wamalwa D, et al. Characterizing provider-led adaptations to mobile phone delivery of the Adolescent Transition Package (ATP) in Kenya using the Framework for Reporting Adaptations and Modifications to Evidence-based Implementation Strategies (FRAME-IS): a mixed methods approach. Implement Sci Commun. 2023;4: 95. https://doi.org/10.1186/s43058-023-00446-y.
Google Scholar
Siegel A, Zuo Y, Moghaddamcharkari N, McIntyre RS, Rosenblat JD. Barriers, benefits and interventions for improving the delivery of telemental health services during the coronavirus disease 2019 pandemic: a systematic review. Curr Opin Psychiatry. 2021. https://doi.org/10.1097/YCO.0000000000000714.
Google Scholar
Galvin E, Desselle S, Gavin B, Quigley E, Flear M, Kilbride K, et al. Patient and provider perspectives of the implementation of remote consultations for community-dwelling people with mental health conditions: a systematic mixed studies review. J Psychiatr Res. 2022. https://doi.org/10.1016/j.jpsychires.2022.10.051.
Google Scholar
Ninsiima LR, Chiumia IK, Ndejjo R. Factors influencing access to and utilisation of youth-friendly sexual and reproductive health services in sub-Saharan Africa: a systematic review. Reprod Health. 2021. https://doi.org/10.1186/s12978-021-01183-y.
Google Scholar
Napierala Mavedzenge SM, Doyle AM, Ross DA. Hiv prevention in young people in sub-Saharan Africa: a systematic review. J Adolesc Health. 2011. https://doi.org/10.1016/j.jadohealth.2011.02.007.
Google Scholar
Mwale M, Muula AS. Systematic review: a review of adolescent behavior change interventions [BCI] and their effectiveness in HIV and AIDS prevention in sub-Saharan Africa. BMC Public Health. 2017. https://doi.org/10.1186/s12889-017-4729-2.
Google Scholar
Mbunge E, Batani J, Gaobotse G, Muchemwa B. Virtual healthcare services and digital health technologies deployed during coronavirus disease 2019 (COVID-19) pandemic in South Africa: a systematic review. Global Health Journal. 2022. https://doi.org/10.1016/j.glohj.2022.03.001.
Google Scholar
L’Engle KL, Mangone ER, Parcesepe AM, Agarwal S, Ippoliti NB. Mobile phone interventions for adolescent sexual and reproductive health: a systematic review. Pediatrics. 2016. https://doi.org/10.1542/peds.2016-0884.
Google Scholar
Janighorban M, Boroumandfar Z, Pourkazemi R, Mostafavi F. Barriers to vulnerable adolescent girls’ access to sexual and reproductive health. BMC Public Health. 2022. https://doi.org/10.1186/s12889-022-14687-4.
Google Scholar
Akinfaderin-Agarau F, Chirtau M, Ekponimo S, Power S. Opportunities and limitations for using new media and mobile phones to expand access to sexual and reproductive health information and services for adolescent girls and young women in six Nigerian states. Afr J Reprod Health. 2012;16:219–30.
Google Scholar
Feroz AS, Ali NA, Khoja A, Asad A, Saleem S. Using mobile phones to improve young people sexual and reproductive health in low and middle-income countries: a systematic review to identify barriers, facilitators, and range of mHealth solutions. Reprod Health. 2021. https://doi.org/10.1186/s12978-020-01059-7.
Google Scholar
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013. https://doi.org/10.7448/ias.16.3.18640.
Google Scholar
Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017. https://doi.org/10.2105/AJPH.2017.303744.
Google Scholar
Hogwood J, Campbell T, Butler S. I wish i could tell you but I can’t: adolescents with perinatally acquired HIV and their dilemmas around self-disclosure. Clin Child Psychol Psychiatry. 2013. https://doi.org/10.1177/1359104511433195.
Google Scholar
Mugo C, Kohler P, Kumar M, Badia J, Kibugi J, Wamalwa DC, et al. Individual-, interpersonal- and institutional-level factors associated with HIV stigma among youth in Kenya. AIDS Behav. 2023. https://doi.org/10.1007/s10461-023-03982-9.
Google Scholar