- Temperatures dip amid snowfall in Murree, rain in twin cities Dawn
- Snow, fog disrupt transport nationwide The Express Tribune
- Heavy snowfall forces closure of Murree Expressway Daily Times
- Snowfall in Murree intensifies cold across northern…
Author: admin
-
Temperatures dip amid snowfall in Murree, rain in twin cities – Dawn
-
Labour unions reject amendments to ICT local government law – Dawn
- Labour unions reject amendments to ICT local government law Dawn
- LG elections in capital likely to be postponed again Dawn
- Cabinet clears new local system for Islamabad The Express Tribune
- Cabinet approves key policy decisions as PM reaffirms SOE…
Continue Reading
-
SBP reserves rise $4.2bn in 2025 – Dawn
- SBP reserves rise $4.2bn in 2025 Dawn
- Pakistan’s short-term FX liabilities reach around $31bn Mettis Global
- State Bank of Pakistan Foreign Reserves Rise $16 Million The Daily CPEC
- SBP forex reserves register jump of Rs1.3 crore 24 News HD
- State Bank’s reserves edge up to $15.91b The Express Tribune
Continue Reading
-
Tahir Ashrafi named coordinator for religious harmony – Dawn
- Tahir Ashrafi named coordinator for religious harmony Dawn
- PUC Chairman Tahir Ashrafi appointed liaison for religious harmony, Pakistani diaspora in Muslim countries Dawn
- PM appoints Tahir Ashrafi as coordinator for religious harmony, diaspora in…
Continue Reading
-
Country witnessed 34pc increase in terrorism in 2025 – Dawn
- Country witnessed 34pc increase in terrorism in 2025 Dawn
- Border Closure Brings Down Terrorist Violence Center for Research and Security Studies (CRSS)
- Pakistan’s Worsening Threat Landscape in 2025 The Diplomat – Asia-Pacific Current Affairs…
Continue Reading
-

Top-Seeded Indiana Posts First CFP Victory with 38-3 Rose Bowl Win over No. 9 Alabama
PASADENA, Calif. — Fernando…
Continue Reading
-
Samsung Unveils AI Projector for Corner Projections – 조선일보
- Samsung Unveils AI Projector for Corner Projections 조선일보
- Samsung Unveils The Freestyle+ Ahead of CES 2026, Showcasing a Smart AI Portable Screen samsung.com
- Samsung’s fan-favorite portable projector just got a bright refresh Android…
Continue Reading
-
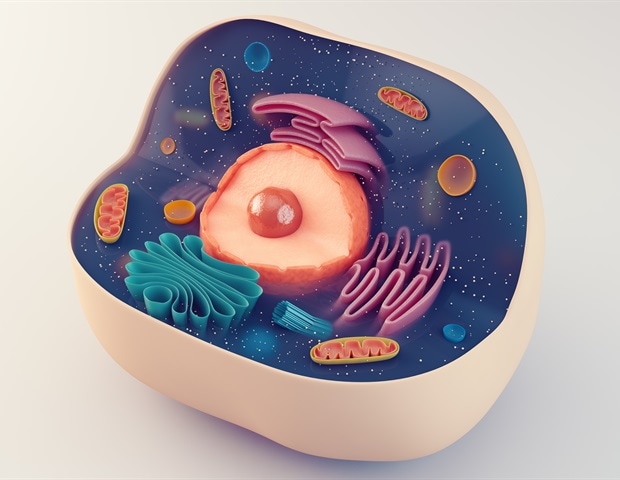
Label-free polarized light reveals subtle red blood cell deformations
Red blood cells are essential for oxygen transport and immune function in the human body. When these cells become abnormally shaped, they can indicate serious health conditions, including diabetes, malaria, hereditary blood…
Continue Reading
-

Gaming, Videos Don’t Cause Inattentiveness. Social Media Does.
Published: January 1, 2026
Photo from Laura Chouette via Unsplash By Michaela Gordoni
A new study found that social media is causing kids’ attention to drop.
Researchers at the Karolinska Institute in Sweden and the Oregon Health & Science…
Continue Reading
-

Before & After: Dated 2000s Kitchen Gets a Striking $2,000 Makeover (The Cabinets Stayed!)
Orange-y wooden cabinets from the ’90s and 2000s might have a bit of a dated look to them, but they can be worth keeping just for the sheer quality of the wood. Throw a little paint on them, and they’ll be perfectly on-trend today, when dark…
Continue Reading