Characterization of mRNA Sequences and Expression of RASA1 in Chicken Embryonic Tissues at E6 and E12
The RASA1 gene is present on both the Z and W sex chromosomes in chickens, referred to as RASA1-Z and RASA1-W, respectively. According to the…

The RASA1 gene is present on both the Z and W sex chromosomes in chickens, referred to as RASA1-Z and RASA1-W, respectively. According to the…
The CHARLS is a prospective national cohort study that enrolled 17,708 participants in 2011, and three waves of follow-up were conducted in 2013, 2015, and 2018. Participants were randomly selected using a probability-proportional-to-size (PPS) technique and a four-stage random sample method. The workgroup selected 150 counties in 28 provinces. Administrative villages in rural areas and neighborhoods in urban areas were the primary sampling units (PSUs). Three PSUs within each county-level unit were selected using PPS sampling. Detailed information on the methodology and cohort profile has been reported previously [11].
We collected data on participants enrolled in the baseline investigation who attended all three follow-up investigations and aged above 60 years old. Those with a history of cancer were excluded because the progression and treatment of cancer affect multiple organs and systems throughout the body; this aspect could have introduced substantial bias into our study. During the data cleaning process, we identified participants with implausible data regarding body weight and height, specifically heights less than 100 cm or weights less than 20 kg. These values were considered erroneous owing to likely data entry mistakes; therefore, participants with an abnormal body mass index (BMI) (BMI < 10 or BMI > 60) in the baseline investigation were excluded.
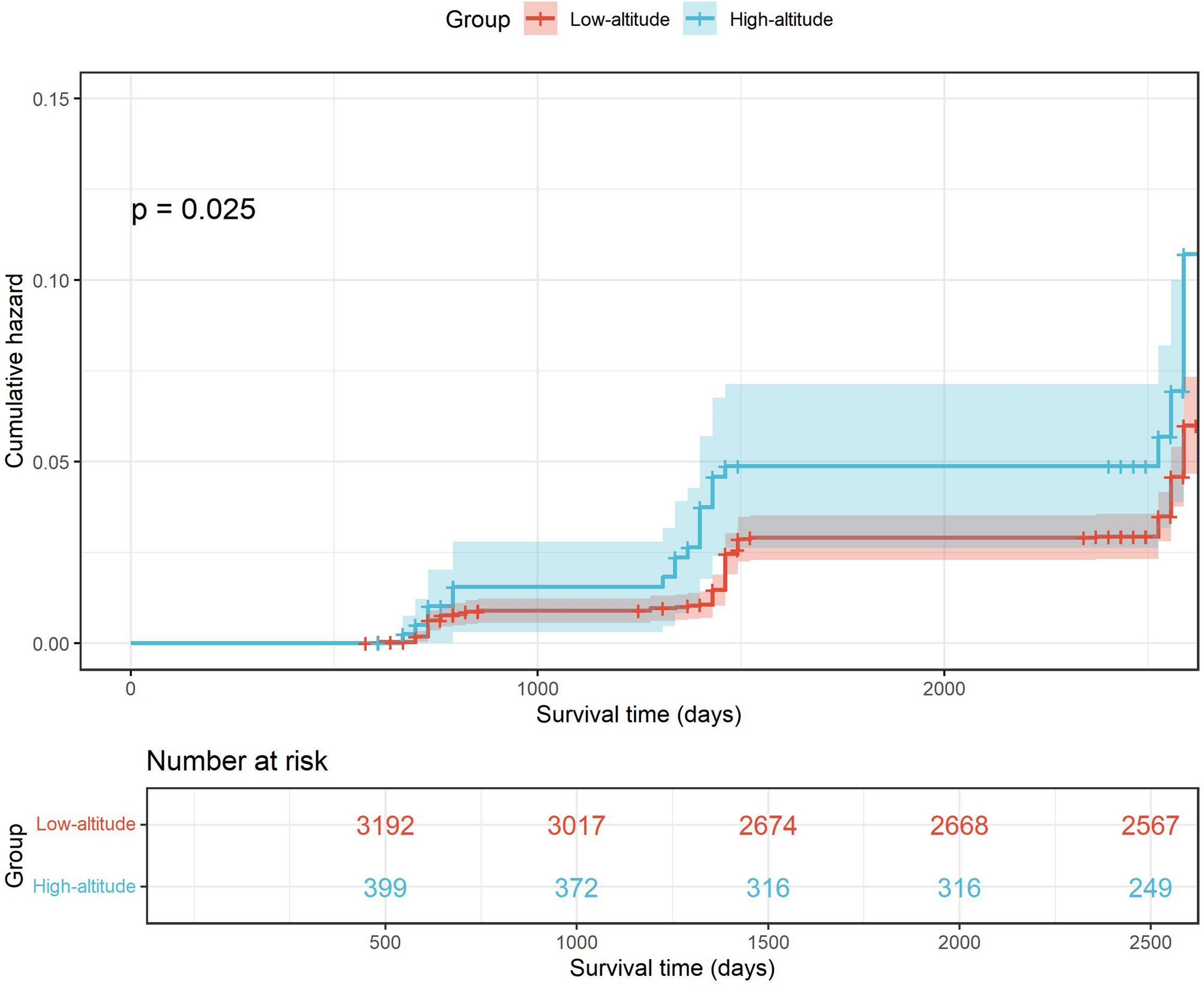
The participants’ place of residence was determined by their community ID. The latitude and longitude were acquired through amap api (https://restapi.amap.comv3/geocode), and the local altitude was acquired based on the latitude and longitude using geodata (version 0.5-8) [12] packages and the raster package (version 3.6–23) [13]. Participants were stratified into a low-altitude or high-altitude group based on a criterion of 1500 m, which was used in previous studies [14].
The primary outcome was hip fractures reported by the participants, which was defined by their answer to the question, “Have you fractured your hip since the last interview?” Participants choosing “yes” were considered to have experienced a hip fracture, and the time point the investigation occurred was recorded as the time the event happened.
Individual income, marital status, medical history, sex, BMI, smoking status, alcohol consumption, and age were selected as covariates for propensity score matching (PSM). Individual income was acquired from harmonized CHARLS data and evenly divided into five groups. Educational status was retrieved from the answer to the question: “What is the highest level of education completed?” and re-coded into preschool, primary, secondary, and higher education. Marital status was retrieved from the answer to the question: “What is your marital status?” and re-coded as unmarried, married, widowed, divorced (or long-term separation). History of stroke, cardiovascular dysfunction, falls, hip fractures, chronic lung diseases, and arthritis were retrieved from the answer to the question: “Have you been diagnosed with any of the following by a doctor?” The presence of specific diseases was determined based on whether the participant selected “Yes” to the following conditions: (1) “Chronic lung diseases, such as chronic bronchitis and emphysema (excluding tumors or cancer),” (2) “Heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems,” (3) “Stroke,” and (4) “Arthritis or rheumatism.” BMI was calculated using the following formula: BMI (kg/m[2]) = body weight (kg)/body height (m)2.
Individual income, marital status, medical history, sex, BMI, smoking status, alcohol consumption, and age were selected for PSM. A general linear model was used to calculate the distance, and the nearest method was used for matching with a matching ratio of 1:8 (high altitude: low altitude). After matching, a balance test was performed to evaluate the imbalance between the two groups in the matched data. The MatchIt package [15] was used for matching, and the Cobalt package [16] was used for the balanced test and plotting.
Categorical variables are shown as counts (percentages, %), and continuous variables are shown as mean ± SD. To compare the differences in baseline data between the two groups, chi-square and t-tests were used for categorical and continuous variables, respectively. Kaplan–Meier survival analysis and Cox regression were used to compare the differences between the two groups regarding fall and hip fracture risks.
Subgroup analysis was performed, and the participants were divided into subgroups according to sex, smoking history, and overweight status. The effects of high-altitude exposure on fall and hip fracture risks in different subgroups were evaluated using Cox regression analysis.
To test the robustness of our results, we performed different sensitivity analyses as follows: (1) We randomly sampled 80% and 90% of all participants, respectively, and replicated the previously described analysis workflow. (2) Using optimal matching as the PSM method and a matching ratio of 1:8, we replicated the previously described analysis workflow. (3) Cox regression was performed with and without adjustments for covariates without matching the participants.
All analyses were performed using R (version 4.3.1). The survival analysis was performed using the survival package (version 3.5-5) [17] and visualized using the Survminer package (version 0.4.9) [18]. The comparison of baseline characteristics and the generation of tables was performed using the gtsummary package (version 1.7.2) [19].

It’s a good idea to look for Black Friday Apple deals this time of year if you’re thinking about upgrading an aging laptop or picking up a pair of AirPods or an Apple Watch as a gift. One of the best discounts we’re tracking at the moment is on…

Chronic obstructive pulmonary disease (COPD) is a common chronic non-communicable disease among the elderly. Its main pathological feature is persistent airflow limitation caused by abnormal alveolar structures and bronchial…
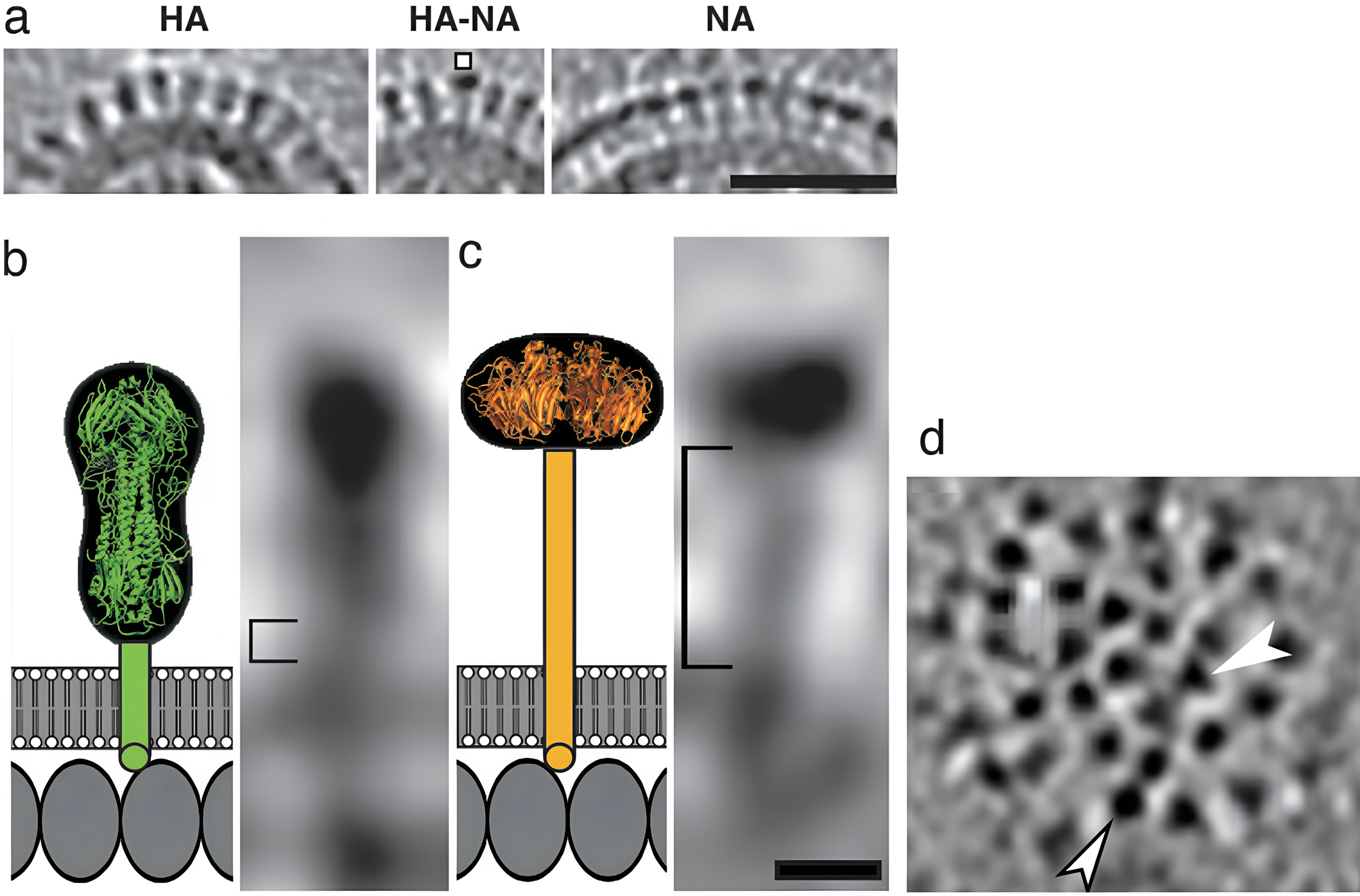
This section describes the experimental dataset, the reconstruction of influenza B virus (B/Lee/40) particles from cryo-EM tilt series, and the computational pipeline for spike segmentation, feature extraction, and classification. These methods…

After two years of brutal warfare in Gaza, a fragile ceasefire – the first phase of US president Donald Trump’s 20-point plan – offers some respite to an exhausted population. For my Unrwa colleagues on the ground in Gaza, the constant fear…
World Health Organization. Guidelines for the psychosocially assisted Pharmacological treatment of opioid dependence. Geneva, Switzerland: World Health Organization; 2009. p. 9241547545. Report No.
Bruneau J, Ahamad K, Goyer M-È, Poulin G, Selby P, Fischer B, et al. Management of opioid use disorders: A National clinical practice guideline. Can Med Assoc J. 2018;190(9):E247–57.
Google Scholar
Priest KC, Gorfinkel L, Klimas J, Jones AA, Fairbairn N, McCarty D. Comparing Canadian and united States opioid agonist therapy policies. Int J Drug Policy. 2019;74:257–65.
Google Scholar
Eibl JK, Morin K, Leinonen E, Marsh DC. The state of opioid agonist therapy in Canada 20 years after federal oversight. Can J Psychiatry Revue Canadienne De Psychiatrie. 2017;62(7):444–50.
Google Scholar
Piske M, Zhou H, Min JE, Hongdilokkul N, Pearce LA, Homayra F, et al. The cascade of care for opioid use disorder: A retrospective study in British Columbia, Canada. Addiction. 2020;115(8):1482–93.
Google Scholar
Tahsin F, Morin KA, Vojtesek F, Marsh DC. Measuring treatment attrition at various stages of engagement in opioid agonist treatment in Ontario Canada using a cascade of care framework. BMC Health Serv Res. 2022;22(1):490.
Google Scholar
O’Connor AM, Cousins G, Durand L, Barry J, Boland F. Retention of patients in opioid substitution treatment: A systematic review. PLoS ONE. 2020;15(5):e0232086.
Google Scholar
Fischer B. The continuous opioid death crisis in canada: changing characteristics and implications for path options forward. Lancet Reg Health – Americas. 2023;19:100437.
Google Scholar
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550.
Google Scholar
Hall NY, Le L, Majmudar I, Mihalopoulos C. Barriers to accessing opioid substitution treatment for opioid use disorder: A systematic review from the client perspective. Drug Alcohol Depend. 2021;221:108651.
Google Scholar
Lachapelle É, Archambault L, Blouin C, Perreault M. Perspectives of people with opioid use disorder on improving addiction treatments and services. Drugs: Educ Prev Policy. 2021;28(4):316–27.
Pearce LA, Min JE, Piske M, Zhou H, Homayra F, Slaunwhite A, et al. Opioid agonist treatment and risk of mortality during opioid overdose public health emergency: population based retrospective cohort study. BMJ. 2020;368:m772.
Google Scholar
Mackay L, Kerr T, Fairbairn N, Grant C, Milloy MJ, Hayashi K. The relationship between opioid agonist therapy satisfaction and Fentanyl exposure in a Canadian setting. Addict Sci Clin Pract. 2021;16(1):26.
Google Scholar
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Google Scholar
Greene SM, Tuzzio L, Cherkin D. A framework for making patient-centered care front and center. Permanente J. 2012;16(3):49.
Google Scholar
Kitson A, Marshall A, Bassett K, Zeitz K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs. 2012;69(1):4–15.
Google Scholar
Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness – A systematic review and concept analysis. PLoS ONE. 2014;9(9):e107828.
Google Scholar
Marchand K, Beaumont S, Westfall J, MacDonald S, Harrison S, Marsh DC, et al. Conceptualizing patient-centered care for substance use disorder treatment: findings from a systematic scoping review. Subst Abuse Treat Prev Policy. 2019;14(1):37.
Google Scholar
Brothers TD, Bonn M. Patient-centred care in opioid agonist treatment could improve outcomes. Can Med Assoc J. 2019;191(17):E460–1.
Google Scholar
British Columbia Centre on Substance Use BMoH, and BC Ministry of Mental Health and Addictions. A guideline for the clinical management of opioid use disorder. Vancouver, BC: British Columbia Centre on Substance Use (BCCSU); 2023.
Rastegar DA. Patient-Centered care in opioid use disorder treatment. In: Wakeman SE, Rich JD, editors. Treating opioid use disorder in general medical settings. Cham: Springer International Publishing; 2021. pp. 1–7.
Edland-Gryt M, Skatvedt AH. Thresholds in a low-threshold setting: an empirical study of barriers in a centre for people with drug problems and mental health disorders. Int J Drug Policy. 2013;24(3):257–64.
Google Scholar
Biancarelli DL, Biello KB, Childs E, Drainoni M, Salhaney P, Edeza A, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2019;198:80–6.
Google Scholar
Harris M, Rhodes T, Martin A. Taming systems to create enabling environments for HCV treatment: negotiating trust in the drug and alcohol setting. Soc Sci Med. 2013;83:19–26.
Google Scholar
Treloar C, Rance J, Yates K, Mao L. Trust and people who inject drugs: the perspectives of clients and staff of needle syringe programs. Int J Drug Policy. 2016;27:138–45.
Google Scholar
Farrugia A, Pienaar K, Fraser S, Edwards M, Madden A. Basic care as exceptional care: addiction stigma and consumer accounts of quality healthcare in Australia. Health Sociol Rev. 2021;30(2):95–110.
Google Scholar
Fraser S, Moore D, Farrugia A, Edwards M, Madden A. Exclusion and hospitality: the subtle dynamics of stigma in healthcare access for people emerging from alcohol and other drug treatment. Sociol Health Illn. 2020;42(8):1801–20.
Google Scholar
Muncan B, Walters SM, Ezell J, Ompad DC. They look at Us like junkies: influences of drug Use stigma on the healthcare engagement of people who inject drugs in new York City. Harm Reduct J. 2020;17(1):53.
Google Scholar
Addison M, Lhussier M, Bambra C. Relational stigma as a social determinant of health: i’m not what you _____see me as. SSM – Qualitative Res Health. 2023;4:100295.
Google Scholar
Marshall K, Maina G, Sherstobitoff J. Plausibility of patient-centred care in high-intensity methadone treatment: reflections of providers and patients. Addict Sci Clin Pract. 2021;16(1):42.
Google Scholar
Treloar C, Rance J, Backmund M. Understanding barriers to hepatitis C virus care and stigmatization from a social perspective. Clin Infect Dis. 2013;57(Suppl 2):S51–5.
Google Scholar
Heller D, McCoy K, Cunningham C. An invisible barrier to integrating HIV primary care with harm reduction services: philosophical clashes between the harm reduction and medical models. Public Health Rep. 2004;119(1):32–9.
Google Scholar
Denis-Lalonde D, Lind C, Estefan A. Beyond the buzzword: A concept analysis of harm reduction. Res Theory Nurs Pract. 2019;4:310–23.
Google Scholar
Frankeberger J, Gagnon K, Withers J, Hawk M. Harm reduction principles in a street medicine program: A qualitative study. Culture. Med Psychiatry. 2023;47(4):1005–21.
Google Scholar
McNeil R, Kerr T, Pauly B, Wood E, Small W. Advancing patient-centered care for structurally vulnerable drug-using populations: A qualitative study of the perspectives of people who use drugs regarding the potential integration of harm reduction interventions into hospitals. Addiction. 2016;111(4):685–94.
Google Scholar
McNeil R, Small W. Safer environment interventions’: A qualitative synthesis of the experiences and perceptions of people who inject drugs. Soc Sci Med. 2014;106:151–8.
Google Scholar
Jakubowski A, Rath C, Harocopos A, Wright M, Welch A, Kattan J, et al. Implementation of buprenorphine services in NYC syringe services programs: A qualitative process evaluation. Harm Reduct J. 2022;19(1):75.
Google Scholar
Latour B, Venn C. Morality and Technology. Theory. Cult Soc. 2002;19(5–6):247–60.
Google Scholar
Fomiatti R, Shaw F, Fraser S. It’s a different way to do medicine’: exploring the affordances of telehealth for hepatitis C healthcare. Int J Drug Policy. 2022;110:103875.
Google Scholar
Høj SB, de Montigny C, Chougar S, Léandre R, Beauchemin-Nadeau M-È, Boyer-Legault G, et al. Co-constructing a community-based telemedicine program for people with opioid use disorder during the COVID-19 pandemic: lessons learned and implications for future service delivery. JMIR Public Health Surveillance. 2023;9:e39236.
Google Scholar
Jauffret-Roustide M, Bertrand K. COVID-19, usages de drogues et réduction des risques: analyse croisée des expériences et de l’impact de La pandémie En France et Au Québec. Criminologie. 2022;55(2):17–42.
Google Scholar
Minoyan N, Høj SB, Zolopa C, Vlad D, Bruneau J, Larney S. Self-reported impacts of the COVID-19 pandemic among people who use drugs: A rapid assessment study in Montreal, Canada. Harm Reduct J. 2022;19(1):38.
Google Scholar
Zolopa C, Brothers TD, Leclerc P, Mary J-F, Morissette C, Bruneau J, et al. Changes in supervised consumption site use and emergency interventions in Montréal, Canada in the first twelve months of the COVID-19 pandemic: an interrupted time series study. Int J Drug Policy. 2022;110:103894.
Google Scholar
Ali F, Russell C, Nafeh F, Rehm J, LeBlanc S, Elton-Marshall T. Changes in substance supply and use characteristics among people who use drugs (PWUD) during the COVID-19 global pandemic: A National qualitative assessment in Canada. Int J Drug Policy. 2021;93:103237.
Google Scholar
Russell C, Ali F, Nafeh F, Rehm J, LeBlanc S, Elton-Marshall T. Identifying the impacts of the COVID-19 pandemic on service access for people who use drugs (PWUD): A National qualitative study. J Subst Abuse Treat. 2021;129:108374.
Google Scholar
Imtiaz S, Nafeh F, Russell C, Ali F, Elton-Marshall T, Rehm J. The impact of the novel coronavirus disease (COVID-19) pandemic on drug overdose-related deaths in the United States and Canada: a systematic review of observational studies and analysis of public health surveillance data. Substance Abuse Treat Prevent Policy. 2021;16(1):87.
Krawczyk N, Fawole A, Yang J, Tofighi B. Early innovations in opioid use disorder treatment and harm reduction during the COVID-19 pandemic: a scoping review. Addict Sci Clin Pract. 2021;16(1):68.
Google Scholar
Alami H, Lehoux P, Attieh R, Fortin J-P, Fleet R, Niang M, et al. A not so quiet revolution: systemic benefits and challenges of telehealth in the context of COVID-19 in Quebec (Canada). Front Digit Health. 2021;3:721898.
Google Scholar
Glegg S, McCrae K, Kolla G, Touesnard N, Turnbull J, Brothers TD, et al. COVID just kind of opened a can of whoop-ass: the rapid growth of safer supply prescribing during the pandemic documented through an environmental scan of addiction and harm reduction services in Canada. Int J Drug Policy. 2022;106:103742.
Google Scholar
Letter from the Minister of Health regarding treatment and safer supply [press release]. Ottawa, ON: Government of Canada, 24 August 2020.
Brar R, Bruneau J, Butt P, Goyer M, Lim R, Poulin G, et al. Medications and other clinical approaches to support physical distancing for people who use substances during the COVID-19 pandemic: National rapid guidance document. Vancouver, BC: Canadian Research Initiative in Substance Misuse; 2020.
Bruneau J, Rehm J, Wild TC, Wood E, Sako A, Swansburg J, Lam A. Telemedicine support for addiction services: National rapid guidance document. Montreal, QC: Canadian Research Initiative in Substance Misuse; 2020.
Health Canada. Subsection 56(1) class exemption for patients, practitioners and pharmacists prescribing and providing controlled substances in Canada Ottawa, ON: Government of Canada. 2020. https://www.canada.ca/en/health-canada/services/health-concerns/controlled-substances-precursor-chemicals/policy-regulations/policy-documents/section-56-1-class-exemption-patients-pharmacists-practitioners-controlled-substances-covid-19-pandemic.html. Accessed 1 Nov 2021.
Goyer M-È, Hudon K, Plessis-Bélair M-C, Ferguson Y. Substance replacement therapy in the context of the COVID-19 pandemic in Québec: clinical guidance for prescribers. Montreal, QC: Institut universitaire Sur les dépendances (IUD); 2020. https://dependanceitinerance.ca/app/uploads/2020/10/Guide-Pharmaco-COVID_ANG-VF.19.10.20.pdf. Accessed 10 Oct 2023.
Collège des médecins du Québec. Trouble lié à l’utilisation d’opioïdes (TUO): Prescription d’un traitement par agonistes opioïdes (TAO) durant la pandémie Montreal, QC: Collège des médecins du Québec. 2020. http://www.cmq.org/page/fr/covid-19-trouble-lie-a-l-utilisation-d-opioides-tuo-prescription-d-un-traitement-par-agonistes-opioides-tao-durant-la-pandemie.aspx. Accessed 8 Apr 2020.
Collège des médecins du Québec. Les téléconsultations réalisées par les médecins durant la pandémie de COVID-19: Guide à l’intention des médecins. Montreal, QC: Collège des médecins du Québec; 31 March 2020. Accessed 11 May 2020.
Mignacca FG. Montreal’s CACTUS safe-injecting community group sees more overdoses amid pandemic Montreal, QC: CBC News; 2020. Accessed 19 Jun 2024. https://www.cbc.ca/news/canada/montreal/cactus-montreal-opioid-overdoses-covid-19-1.5618901
Nosyk B, Min JE, Pearce LA, Zhou H, Homayra F, Wang L, et al. Development and validation of health system performance measures for opioid use disorder in British Columbia, Canada. Drug Alcohol Depend. 2022;233:109375.
Google Scholar
Kurz M, Min JE, Dale LM, Nosyk B. Assessing the determinants of completing OAT induction and long-term retention: A population-based study in British Columbia, Canada. J Subst Abuse Treat. 2022;133:108647.
Google Scholar
Krebs E, Homayra F, Min JE, MacDonald S, Gold L, Carter C, Nosyk B. Characterizing opioid agonist treatment discontinuation trends in British Columbia, Canada, 2012–2018. Drug Alcohol Depend. 2021;225:108799.
Google Scholar
Nielsen S, Degenhardt L, Hoban B, Gisev N. A synthesis of oral morphine equivalents (OME) for opioid utilisation studies. Pharmacoepidemiol Drug Saf. 2016;25(6):733–7.
Patterson Silver Wolf DA, Gold M. Treatment resistant opioid use disorder (TROUD): Definition, rationale, and recommendations. J Neurol Sci. 2020;411:116718.
Google Scholar
Kimmel S, Bach P, Walley AY. Comparison of treatment options for refractory opioid use disorder in the united States and canada: A narrative review. J Gen Intern Med. 2020;35(8):2418–26.
Google Scholar
Voon P, Joe R, Fairgrieve C, Ahamad K. Treatment of opioid use disorder in an innovative community-based setting after multiple treatment attempts in a woman with untreated HIV. BMJ Case Rep. 2016;2016:bcr2016215557.
Håkansson Eklund J, Holmström IK, Kumlin T, Kaminsky E, Skoglund K, Höglander J, et al. Same same or different? A review of reviews of person-centered and patient-centered care. Patient Educ Couns. 2019;102(1):3–11.
Google Scholar
Marlatt GA, Blume AW, Parks GA. Integrating harm reduction therapy and traditional substance abuse treatment. J Psychoactive Drugs. 2001;33(1):13–21.
Google Scholar
Chang JE, Lindenfeld Z, Hagan H. Integrating harm reduction into medical care: lessons from three models. J Am Board Fam Med. 2023;36(3):449–61.
Google Scholar
Salvalaggio G, McKim R, Taylor M, Wild TC. Patient–provider rapport in the health care of people who inject drugs. SAGE Open. 2013;3(4):2158244013509252.
Google Scholar
Lilly R, Quirk A, Rhodes T, Stimson GV. Sociality in methadone treatment: Understanding methadone treatment and service delivery as a social process. Drugs: Educ Prev Policy. 2000;7(2):163–78.
Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–39.
Google Scholar
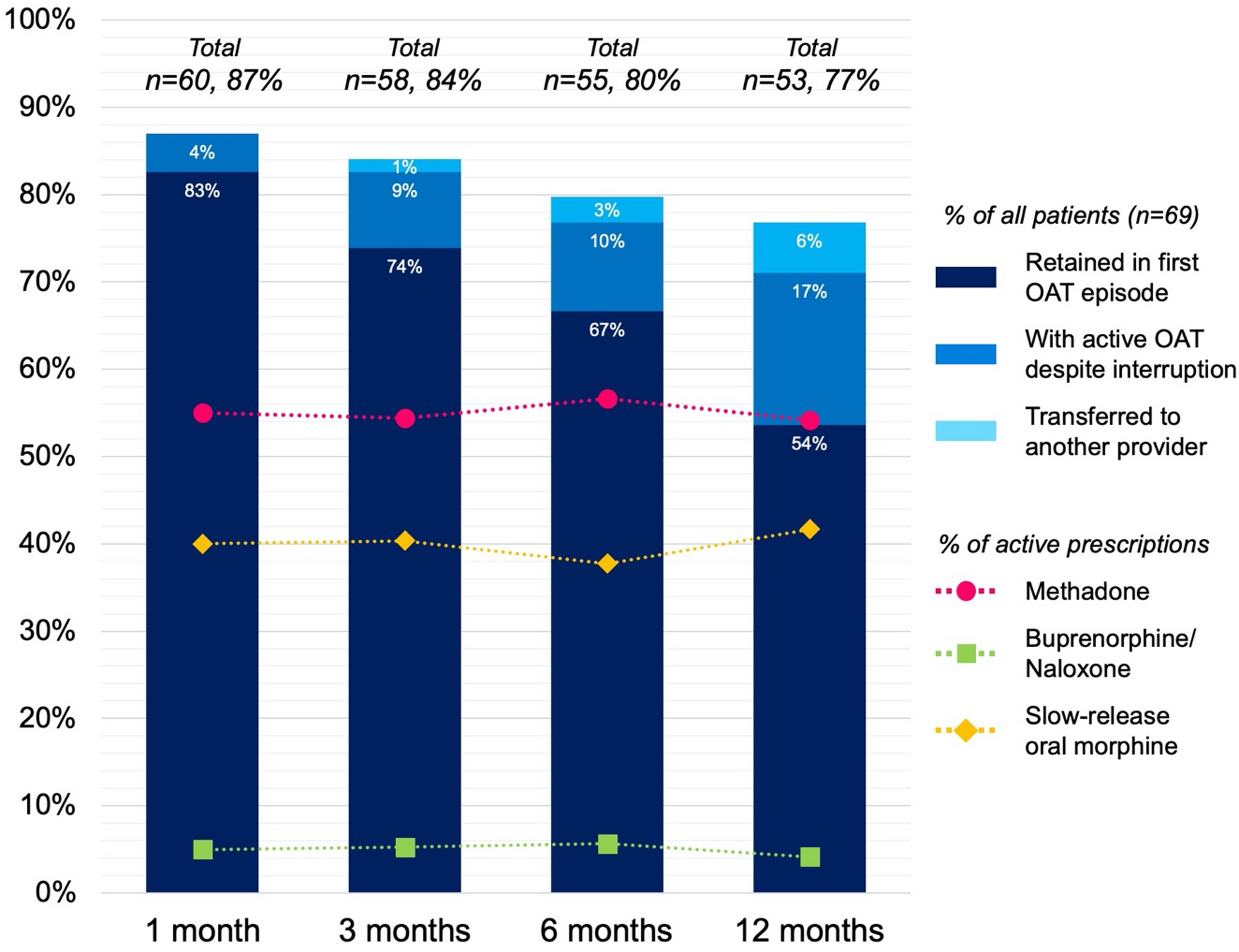
Morin KA, Tatangelo M, Marsh D. Canadian addiction treatment centre (CATC) opioid agonist treatment cohort in Ontario, Canada. BMJ Open. 2024;14(2):e080790.
Google Scholar
Vogel M, Dürsteler KM, Walter M, Herdener M, Nordt C. Rethinking retention in treatment of opioid dependence: the eye of the beholder. Int J Drug Policy. 2017;39:109–13.
Google Scholar
Santo T Jr, Clark B, Hickman M, Grebely J, Campbell G, Sordo L, et al. Association of opioid agonist treatment with All-Cause mortality and specific causes of death among people with opioid dependence: A systematic review and Meta-analysis. JAMA Psychiatry. 2021;78(9):979–93.
Google Scholar
Nosyk B, MacNab YC, Sun H, Fischer B, Marsh DC, Schechter MT, Anis AH. Proportional hazards frailty models for recurrent methadone maintenance treatment. Am J Epidemiol. 2009;170(6):783–92.
Google Scholar
Pilarinos A, Kwa Y, Joe R, Thulien M, Buxton JA, DeBeck K, Fast D. Navigating opioid agonist therapy among young people who use illicit opioids in Vancouver, Canada. Int J Drug Policy. 2022;107:103773.
Google Scholar
Bell J, Burrell T, Indig D, Gilmour S. Cycling in and out of treatment: participation in methadone treatment in NSW, 1990–2002. Drug Alcohol Depend. 2006;81(1):55–61.
Google Scholar
Nordt C, Vogel M, Dey M, Moldovanyi A, Beck T, Berthel T, et al. One size does not fit all—evolution of opioid agonist treatments in a naturalistic setting over 23 years. Addiction. 2019;114(1):103–11.
Google Scholar
Muller AE, Bjørnestad R, Clausen T. Dissatisfaction with opioid maintenance treatment partly explains reported side effects of medications. Drug Alcohol Depend. 2018;187:22–8.
Google Scholar
Giang K, Charlesworth R, Thulien M, Mulholland A, Barker B, Brar R, et al. Risk mitigation guidance and safer supply prescribing among young people who use drugs in the context of COVID-19 and overdose emergencies. Int J Drug Policy. 2023;115:104023.
Google Scholar
Min JE, Guerra-Alejos BC, Yan R, Palis H, Barker B, Urbanoski K, et al. Opioid coprescription through risk mitigation guidance and opioid agonist treatment receipt. JAMA Netw Open. 2024;7(5):e2411389–e.
Google Scholar
Sanders JJ, Roose RJ, Lubrano MC, Lucan SC. Meaning and methadone: patient perceptions of methadone dose and a model to promote adherence to maintenance treatment. J Addict Med. 2013;7(5):307–13.
Roux P, Lions C, Michel L, Cohen J, Mora M, Marcellin F, et al. Predictors of non-adherence to methadone maintenance treatment in opioid-dependent individuals: implications for clinicians. Curr Pharm Design. 2014;20(25):4097–105.
Google Scholar
Artenie AA, Minoyan N, Jacka B, Høj S, Jutras-Aswad D, Roy É, et al. Opioid agonist treatment dosage and patient-perceived dosage adequacy, and risk of hepatitis C infection among people who inject drugs. Can Med Assoc J. 2019;191(17):E462–8.
Google Scholar
Hämmig R, Köhler W, Bonorden-Kleij K, Weber B, Lebentrau K, Berthel T, et al. Safety and tolerability of slow-release oral morphine versus methadone in the treatment of opioid dependence. J Subst Abuse Treat. 2014;47(4):275–81.
Google Scholar
Kastelic A, Dubajic G, Strbad E. Slow-release oral morphine for maintenance treatment of opioid addicts intolerant to methadone or with inadequate withdrawal suppression. Addiction. 2008;103(11):1837–46.
Google Scholar
Yarborough BJH, Stumbo SP, McCarty D, Mertens J, Weisner C, Green CA. Methadone, buprenorphine and preferences for opioid agonist treatment: A qualitative analysis. Drug Alcohol Depend. 2016;160:112–8.
Google Scholar
Mocanu V, Bozinoff N, Wood E, Jutras-Aswad D, Le Foll B, Lim R, et al. Opioid agonist therapy switching among individuals with prescription-type opioid use disorder: secondary analysis of a pragmatic randomized trial. Drug Alcohol Depend. 2023;248:109932.
Google Scholar
Saxon AJ. Short-acting, full agonist opioids during initiation of opioid agonist treatment in the Fentanyl era. JAMA Netw Open. 2024;7(5):e2411398–e.
Google Scholar
Behnia B. Trust development: A discussion of three approaches and a proposed alternative. Br J Social Work. 2007;38(7):1425–41.
Google Scholar
Fine GA. Agency, structure, and comparative contexts: toward a synthetic interactionism. Symbolic Interact. 1992;15(1):87–107.
Google Scholar
Rance J, Newland J, Hopwood M, Treloar C. The politics of place(ment): problematising the provision of hepatitis C treatment within opiate substitution clinics. Soc Sci Med. 2012;74(2):245–53.
Google Scholar
Harris J, McElrath K. Methadone as social control: institutionalized stigma and the prospect of recovery. Qual Health Res. 2012;22(6):810–24.
Google Scholar
Harris M, Albers E, Swan T. The promise of treatment as prevention for hepatitis C: meeting the needs of people who inject drugs? Int J Drug Policy. 2015;26(10):963–9.
Google Scholar
Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419–39.
Google Scholar
Aung PTZ, Spelman T, Wilkinson AL, Dietze PM, Stoové MA, Hellard ME. Time-to-hepatitis C treatment initiation among people who inject drugs in Melbourne, Australia. Epidemiol Infect. 2023;151:e84.
Google Scholar
Jiang N, Bruneau J, Makarenko I, Minoyan N, Zang G, Høj SB, et al. HCV treatment initiation in the era of universal direct acting antiviral coverage – Improvements in access and persistent barriers. Int J Drug Policy. 2023;113:103954.
Google Scholar
Malme KB, Ulstein K, Finbråten A-K, Wüsthoff LEC, Kielland KB, Hauge J, et al. Hepatitis C treatment uptake among people who inject drugs in Oslo, norway: A registry-based study. Int J Drug Policy. 2023;116:104044.
Google Scholar
Papalamprakopoulou Z, Ntagianta E, Triantafyllou V, Kalamitsis G, Dharia A, Dickerson SS, et al. Breaking the vicious cycle of delayed healthcare seeking for people who use drugs. Harm Reduct J. 2025;22(1):27.
Google Scholar
Cochran G, Bruneau J, Cox N, Gordon AJ. Medication treatment for opioid use disorder and community pharmacy: expanding care during a National epidemic and global pandemic. Subst Abus. 2020;41(3):269–74.
Google Scholar
Fatani S, Bakke D, D’Eon M, El-Aneed A. Qualitative assessment of patients’ perspectives and needs from community pharmacists in substance use disorder management. Subst Abuse Treat Prevent Policy. 2021;16(1):38.
Bishop LD, Rosenberg-Yunger ZRS. Pharmacists expanded role in providing care for opioid use disorder during COVID-19: A qualitative study exploring pharmacists’ experiences. Drug Alcohol Depend. 2022;232:109303.
Google Scholar
Tyndall M. Safer opioid distribution in response to the COVID-19 pandemic. Int J Drug Policy. 2020;83:102880.
Bardwell G, Ivsins A, Wallace JR, Mansoor M, Kerr T. The machine doesn’t judge: counternarratives on surveillance among people accessing a safer opioid supply via biometric machines. Soc Sci Med. 2024;345:116683.
Google Scholar
This request seems a bit unusual, so we need to confirm that you’re human. Please press and hold the button until it turns completely green. Thank you for your cooperation!