Nutrition labels on the front of food packaging should be made mandatory in the UK, according to a consumer champion.
Which? called on the Government to make the change amid what it described as an “obesity crisis”.
A “better…
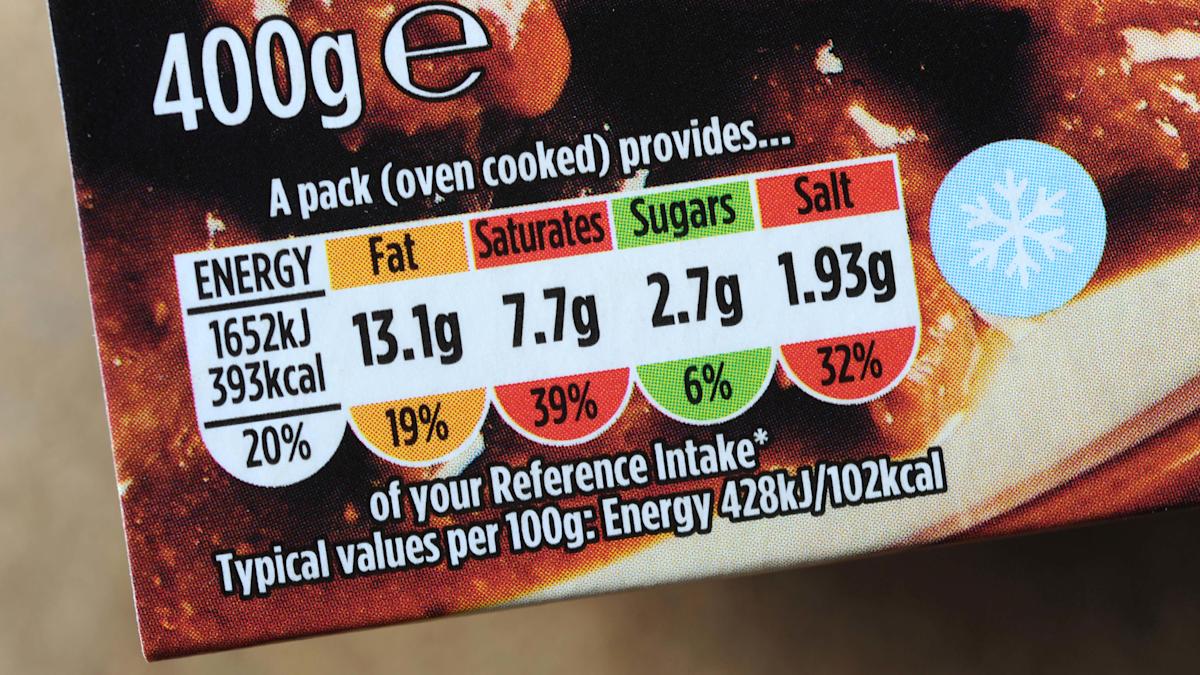
Nutrition labels on the front of food packaging should be made mandatory in the UK, according to a consumer champion.
Which? called on the Government to make the change amid what it described as an “obesity crisis”.
A “better…
Zhao, X. et al. Clinical characteristics and risk factors for Mycoplasma pneumoniae pneumonia in children. Front. Pead. 12, 1438631. https://doi.org/10.3389/fped.2024.1438631 (2024).
Wang, L….
People with hepatitis C virus who inject drugs could be evaluated for cure approximately 2 months earlier than current standards call for.
In a sample of nearly 70 individuals, researchers observed perfect concordance for HCV RNA viral load 4…
![[Press release] Dramatic decline in new cases of orphanhood in Uganda driven by HIV treatment and prevention programs](https://afnnews.qaasid.com/wp-content/uploads/2025/10/350619dc-60db-4a6f-8287-8363a62f487c.jpg)
The scale-up of HIV treatment and prevention programs has led to remarkable declines in orphanhood rates in Rakai, Uganda, according to a new study at Columbia University Mailman…

Bayard “Barney” Clarkson, a pioneering leukemia researcher, a career-long member of the faculty of Memorial Sloan Kettering Cancer Center, and past president of the American Society of Clinical Oncology and the American Association for…
The North Carolina Department of Health and Human Services today announced a new case of measles in Rutherford County. This brings the total number of North Carolina measles cases to five since late December. All individuals who may have been…
![[Press release] ACTG launches IPACE-HIV to study frailty intervention](https://afnnews.qaasid.com/wp-content/uploads/2025/10/clinical-trial-icon-gaac45ea20-1280-scaled.png)
CHAPEL HILL, N.C., Jan. 09, 2026 (GLOBE NEWSWIRE) — ACTG, a global clinical trials network focused on HIV and other infectious diseases, today announced the opening of the IPACE-HIV study (Improving Physical Ability and…

Paul F. Engstrom, a well-respected, longtime member of our Fox Chase Cancer Center community, died Dec. 26. He was 89.
Dr. Engstrom’s story is an impressive one. A world-renowned physician with small-town roots, he helped build a nationally…

Weight restoration is traditionally recognized as the central indicator of recovery in those with anorexia nervosa (AN); however, recent studies are discovering that attaining normal weights may not necessarily reflect full physiologic recovery….

Healthy women with elevated lipoprotein(a) levels are at greater risk of cardiovascular events over…