Introduction
NME is a rare disorder associated with multiple diseases, including glucagonoma, chronic pancreatitis, nutritional deficiency, liver diseases, and inflammatory bowel disease. About 70% of cases of glucagonoma may present with NME, therefore NME is an important visual clue for the diagnosis, enabling timely intervention.
Glucagonoma is an unusual neuroendocrine tumor, derives from the pancreatic alpha cells with an estimated incidence of 1 in 20 million,1 most commonly affecting people in their 50s.2 The main manifestations are weight loss, NME, diabetes, diarrhea, anemia, and neuropsychiatric symptoms. NME is a crucial characteristic of glucagonoma. However, many primary dermatologists lack sufficient knowledge about the disorder, leading to potential misdiagnosis and missed diagnosis. Consequently, we report a case of typical NME combined with glucagonoma diagnosed in 2024 at Dermatology Hospital of Southern Medical University, designed to strengthen the diagnosis and differentiation ability of dermatologists.
Case Presentation
The patient was a 41-year-old male who presented with erythema with erosions on both lower limbs, accompanied by malnutrition and mild itching for the past three years. The patient was diagnosed with “eczema” in the local hospital. He had been treated with topical corticosteroids for years with improvement but frequently recurred. One month ago, the lesions gradually spread all over the body, with crusted papules and polycyclic plaques with a map-like margin mainly involving the face, groin, buttocks, and extremities. And his tongue appeared beefy red and fissuring (Figure 1). No nail abnormality was found.
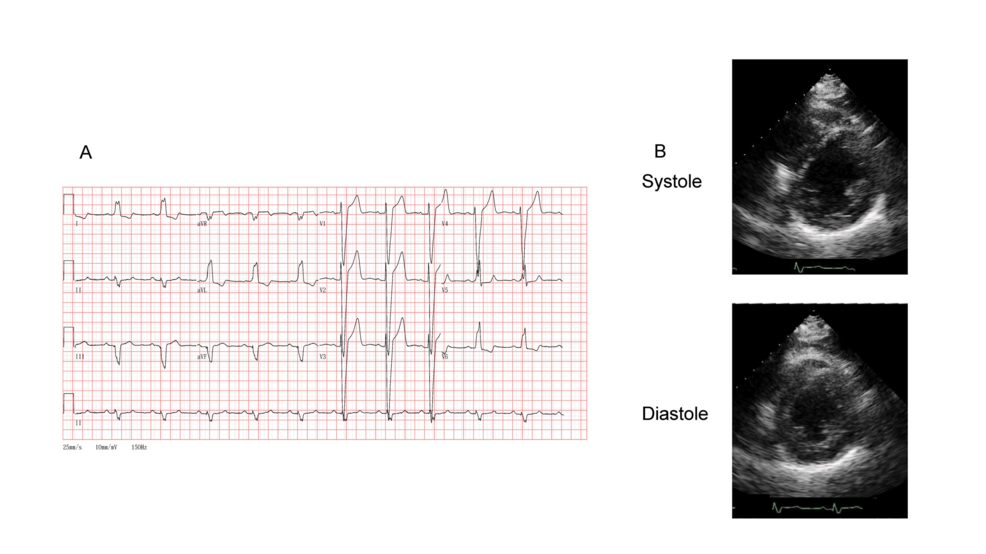
|
Figure 1 Clinical appearance. (a) Scattered erythematous seborrheic plaques on the face. (b) Bright red, swollen tongue; multiple fissures; beefy tongue appearance. (c) Well-defined erythema with raised borders and yellow crusting on both inguinal areas and scrotum. (d and e) Multiple erythema and erosion on the buttocks and knees. (f) Well-defined erythema with raised borders and yellow crusting on both ankles.
|
Laboratory analysis found a serum glucagon level of more than 128 pmol/L (normal range, 2 to 18 pmol/L). Anti-bp180 and anti-bp230, cortisol levels were negative. A skin biopsy was performed and showed parakeratosis, inflammatory crust, spongiosis, localized necrosis in the upper epidermis, lymphocytes infiltrating peri-follicular and peri-vascular areas, and eosinophilic infiltration (Figure 2). A contrast-enhanced abdominal computed tomographic scan revealed an enhancing pancreatic body tail mass and liver metastases (Figure 3).
 |
Figure 2 Histological findings of plaque on the left thigh. Parakeratosis, spongiosis, localized necrosis in the upper epidermis. (HE, x 400).
|
 |
Figure 3 Enhanced abnormal computed tomography scan. Showing a pancreatic body tail mass (right arrow) and intrahepatic mass (left arrow), confirming glucagonoma.
|
Diagnostic Evaluation
The clinical presentation was characteristic of NME, confirmed by histopathological examination of skin biopsy. In accordance with the known correlation between NME and glucagonoma, serum glucagon levels were found to be significantly elevated. Subsequent abdominal CT demonstrated a pancreatic neuroendocrine tumor, establishing the definitive diagnosis of glucagonoma. Therefore, the diagnosis of NME combined with glucagonoma was made.
Treatment with microelements such as zinc, Vitamin B, folic acid, antihistamines, and topical corticosteroids. The rash reduced slightly. However, the patient refused surgical treatment for financial reasons.
Discussion
Glucagonoma is a neuroendocrine tumor characterized by excessive proliferation of α-cells in the pancreas, with a higher prevalence in women than men. The tumor typically grows slowly and can metastasize. Due to the excessive secretion, glucagonoma syndrome occurs, which may present with NME, weight loss, diabetes, diarrhea, anemia, and neuropsychiatric symptoms.3 NME manifests as scaly, erosive, ring-shaped erythema with the formation of pustules and large blisters. Other manifestations may include nail dystrophy, cheilitis, and stomatitis.
Given the rarity of NME, reports on the condition are few both nationally and internationally, and a standardized diagnostic criterion has not yet been made. In 2018, Xuechen Cao and Yan Lu reviewed and summarized previous cases and proposed diagnostic criteria for glucagonoma.4 The primary diagnostic criteria(Table-1) include (1) Imaging revealing a pancreatic mass, (2) Elevated plasma glucagon levels (>1000 ng/L), (3) Typical NME manifestations, (4) A history of multiple endocrine neoplasia. Secondary criteria include (1) New-onset diabetes (fasting plasma glucose, oral glucose tolerance test), (2) low serum zinc levels and hypoaminoacidemia, (3) Unexplained weight loss and diarrhea, (4) Cheilitis or glossitis. In this case, the patient met the primary criteria of (1), (2), and (3), as well as the secondary criterion of (4), confirming the diagnosis of NME associated with glucagonoma.
 |
Table 1 the Diagnostic Criteria and Differential Diagnosis
|
Given its rarity and prolonged clinical course, NME is frequently misdiagnosed as eczema. In such cases, dermatologists should maintain a high clinical suspicion for associated systemic diseases. Several conditions can present with NME-like skin rashes, including Acrodermatitis Enteropathica (AE), pemphigus erythematosus(PE), drug eruption, essential fatty acid deficiency, vitamin deficiency-related dermatitis, and pseudoglucagonoma syndrome.
AE: it is a rare, recessively inherited disorder associated with zinc metabolism abnormalities, typically presenting in infancy with symptoms such as eczema-like dermatitis, crusting, bullae, and pustules, commonly affecting the extremities and perioral areas.5 Additional symptoms include hair loss, diarrhea, stomatitis, photophobia, nail dystrophy, abnormal hair texture, growth retardation, and emotional disorders. Especially common in artificially fed infants, with few in adulthood.6 The serum zinc level is always low.7
PE: the lesions appear as erythematous patches, often found on the face, neck, chest, and other areas, and may have an irregular shape with unclear borders. It may also present in a linear or ring-shaped pattern, with associated vesicles and bullae. Mucosal involvement, such as oral ulcers, throat pain, and ocular inflammation, may also occur. The disease progresses rapidly, with vesicles easily rupturing to form ulcers, and lesions may spread to adjacent skin, occasionally accompanied by secondary infections. Hematoxylin-eosin stain (HE) typically shows superficial epidermal acantholysis, usually located in the granular layer or upper epidermis. Spongiosis and dermal eosinophilic infiltration can be observed, and DIF typically reveals antibodies between epidermal keratinocytes as well as scattered granular deposits of antibodies along the basement membrane zone (BMZ).8
Drug Eruption: it manifests in various clinical forms, with severe reactions presenting as generalized erythema, vesicles, and erosion. Drug eruption usually has a clear history of drug exposure before the onset of the rash, typically resulting from a non-anticipated inflammatory response affecting the skin and/or mucous membranes as a result of drugs entering the body through oral ingestion, inhalation, injection, suppositories, or topical absorption.2 It often shows a clear response to corticosteroid therapy.
The pathogenesis of NME remains unclear. Hyperglucagonemia is believed to play a significant role, because excessive glucagon secretion induces amino acid metabolic dysregulation, culminating in hypoaminoacidemia and consequent impairment of epidermal protein synthesis. And surgical removal of glucagonomas or somatostatin analogs can control the skin rash.6,9 Additionally, hypoaminoacidemia, micronutrient depletion, and deficiencies in essential fatty acids and zinc should also be considered, as nutritional support and topical zinc therapy have been used to improve symptoms.10 Surgical resection is considered the only curative treatment.11 If left untreated, glucagonomas may metastasize to distant organs such as the liver and lungs, leading to progressive clinical deterioration and ultimately life-threatening complications. Surgical options include simple excision (for tumors <2 cm) with regional lymphadenectomy, pancreaticoduodenectomy with regional lymphadenectomy, distal pancreatectomy, and splenectomy. However, over half of glucagonomas are metastatic at diagnosis, with liver metastasis being the most common.12 Liver transplantation is considered a potential treatment for patients with liver metastasis. Transarterial chemoembolization (TACE), radiofrequency ablation, and surgery combined may offer advantages in resecting isolated metastatic tumors. Pharmacological treatments for glucagonoma include chemotherapy, somatostatin analogs, and targeted molecular therapies.13 Molecular targeted therapy: Agents such as sunitinib and everolimus inhibit specific molecular aberrations within tumors, thereby significantly prolonging progression-free survival (PFS).14
Conclusion
NME mainly presents a chronic course, but the recurrent rash seriously affects the patient’s quality of life. The lesions in our case are characterized by generalized erythema with erosions, which are easily misdiagnosed as pemphigus, eczema, and drug eruption, highlighting the importance of precise imaging to exclude pancreatic tumors, when facing similar conditions. Since NME might be the only clue for the early detection of this tumor, it is very important to correctly diagnose. This requires collaborative efforts from dermatologists, endocrinologists, gastroenterologists, and oncologists. This interdisciplinary approach is essential for the timely diagnosis and management of this rare condition. All in all, this case underscores the importance of recognizing NME as a dermatologic marker for systemic malignancies, necessitating collaborative care for timely diagnosis and treatment.
Ethics Statement
The publications of images were included with the patient’s consent.
Consent Statement
The patient had given written informed consent for the publication of his clinical details. Institutional approval is not required for this case study.
Acknowledgments
The authors would like to thank the patient for participation in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by The “Set Sail” Program for Young PhD Researchers in Basic and Applied Medical Research (SL2023A04J02432).
Disclosure
The authors report no conflicts of interest in this work.
References
1. He S, Zeng W, Geng S, Jia J. Glucagonoma syndrome with atypical necrolytic migratory erythema. Indian J Dermatol Venereol Leprol. 2021;87(1):49–53. doi:10.4103/ijdvl.IJDVL_588_18
2. Yang WJ, Hu HH, Guo H, Li JH. Generalized migratory erythema in an elderly woman Necrolytic migratory erythema. J Dtsch Dermatol Ges. 2022;20(2):231–234. doi:10.1111/ddg.14664
3. Liu JW, Qian YT, Ma DL. Necrolytic migratory erythema. JAMA Dermatol. 2019;155(10):1180. doi:10.1001/jamadermatol.2019.1658
4. Cao X, Yan L. 坏死松解性游走性红斑临床研究进展. 中华医学杂志. 2018;98(33):2694–2696. doi:10.3760/cma.j.issn.0376-2491.2018.33.019
5. Maverakis E, Fung MA, Lynch PJ, et al. Acrodermatitis enteropathica and an overview of zinc metabolism. J Am Acad Dermatol. 2007;56(1):116–124. doi:10.1016/j.jaad.2006.08.015
6. van Beek AP, de Haas ER, van Vloten WA, Lips CJ, Roijers JF, Canninga-van Dijk MR. The glucagonoma syndrome and necrolytic migratory erythema: a clinical review. Eur J Endocrinol. 2004;151(5):531–537. doi:10.1530/eje.0.1510531
7. Zou P, Du Y, Yang C, Cao Y. Trace element zinc and skin disorders. Front Med Lausanne. 2022;9:1093868. doi:10.3389/fmed.2022.1093868
8. Hobbs LK, Noland MB, Raghavan SS, Gru AA. Pemphigus erythematosus: a case series from a tertiary academic center and literature review. J Cutan Pathol. 2021;48(8):1038–1050. doi:10.1111/cup.13992
9. Zhang M, Wang S. 胰体尾切除术成功治愈坏死松解性游走性红斑1例. 中国皮肤性病学杂志. 1–5. doi:10.13735/j.cjdv.1001-7089.202402049
10. Chen L, Guo X, Huihui W, Sun W, Ding H. 营养缺乏所致坏死松解性游走性红斑样皮损. 临床皮肤科杂志. 2022;51(05):282–285. doi:10.16761/j.cnki.1000-4963.2022.05.008
11. John AM, Schwartz RA. Glucagonoma syndrome: a review and update on treatment. J Eur Acad Dermatol Venereol. 2016;30(12):2016–2022. doi:10.1111/jdv.13752
12. Adams DR, Miller JJ, Seraphin KE. Glucagonoma syndrome. J Am Acad Dermatol. 2005;53(4):690–691. doi:10.1016/j.jaad.2005.04.071
13. Remes-Troche JM, García-de-acevedo B, Zuñiga-Varga J, Avila-Funes A, Orozco-Topete R. Necrolytic migratory erythema: a cutaneous clue to glucagonoma syndrome. J Eur Acad Dermatol Venereol. 2004;18(5):591–595. doi:10.1111/j.1468-3083.2004.00981.x
14. Öberg K. Management of functional neuroendocrine tumors of the pancreas. Gland Surg. 2018;7(1):20–27. doi:10.21037/gs.2017.10.08