- Bridging Artificial Intelligence and Precision Oncology for Cancer Care Targeted Oncology
- I Used AI to Supplement My Oncology Care—It Reshaped My Treatment Plan The ASCO Post
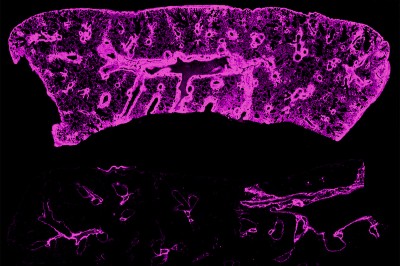
- A I-designed proteins may help spot cancer MIT Technology Review
LA Times The H5N1 bird flu virus that devastated South American elephant seal populations has been confirmed in seals at California’s Año Nuevo State Park, researchers from UC Davis and UC Santa…