‘Peptide detective’ Weizmann immunologist Prof. Yifat Merbl was recognized for a new hidden immune mechanism.



LOS ANGELES — As we indulge in heavier food and alcohol at this time of the year, there’s a hidden holiday danger we should be aware of.
Mix in a little stress, and it may add up to something called “holiday heart syndrome,” which usually refers…

LOS ANGELES — As we indulge in heavier food and alcohol at this time of the year, there’s a hidden holiday danger we should be aware of.
Mix in a little stress, and it may add up to something called “holiday heart syndrome,” which usually refers…

An emergency doctor working at Cork University Hospital said there has been a steady stream of patients of all ages with flu-like symptoms, alongside their regular emergency work, putting pressure on the whole hospital…
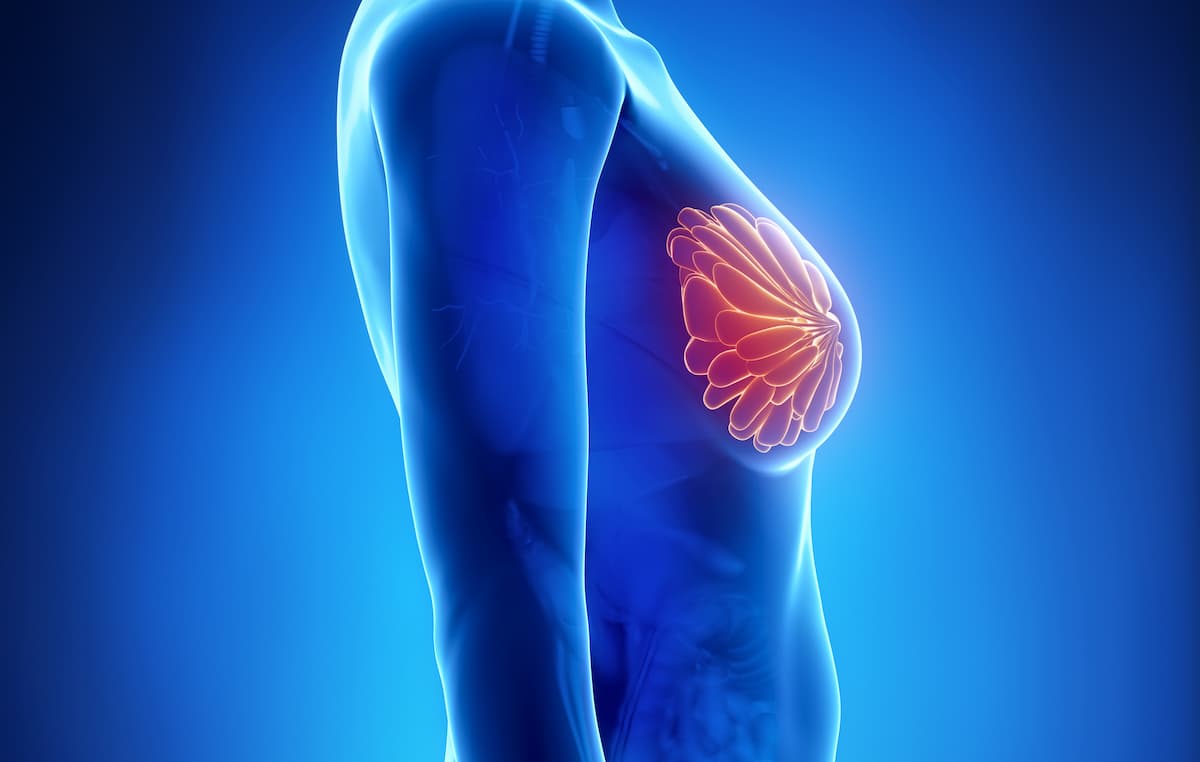
Data from the prospective Premenopausal Breast Cancer Patients’ Fertility Preservation (PREFER) study showed that gonadotropin-releasing hormone agonist (GnRHa) therapy during chemotherapy for early breast cancer was accepted among most…

…

LOS ANGELES (KABC) — As we indulge in heavier food and alcohol at this time of the year, there’s a hidden holiday danger we should be aware of.
Mix in a little stress, and it may add up to something called “holiday heart syndrome,” which usually…

Researchers at the University of Navarra in Spain have created RNACOREX, an open-source software platform designed to identify gene regulation networks linked to cancer survival. The tool was developed by scientists at the Institute of Data…

I’ve had type 1 diabetes for over a decade (I was diagnosed later in life, read my diagnosis story here), and while nothing (no, not even cinnamon or avocado) will miraculously make my pancreas produce insulin on its own, I do have some tricks…
