“I hope this work this will bring equality for people who can’t always access health checks in the same way as the general population,” she added.
Ms Colville said she realised how much harder cancer treatment must be for her former patients…

“I hope this work this will bring equality for people who can’t always access health checks in the same way as the general population,” she added.
Ms Colville said she realised how much harder cancer treatment must be for her former patients…

 BBC
BBCIt is proving difficult to encourage care workers to take the flu vaccine due to myths on social media, the chief executive of the…
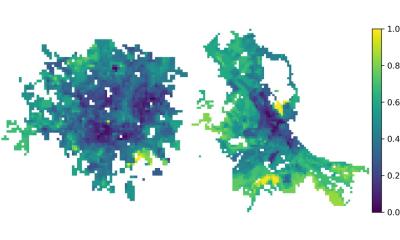
(a–c) Distribution of the population in tiles for the cities under analysis: each tile is coloured according to the number of individuals (see colour bar on the left-hand side). (d) Schematic representation of a tile, with household contacts…

When Heidi Tarr was a teenager, she used a tanning bed several times a week with her friends because they all wanted to glow like a celebrity.
“It was just the thing to do — everyone wanted that nice, dark, tan skin,” the 49-year-old market…

The UK is facing an “unprecedented wave of super flu”, a health chief has warned, as Prime Minister Keir Starmer Friday denounced “reckless” plans by doctors to launch a five-day strike next week.
“The ‘super flu’ epidemic sweeping the country…
Davidov, M. et al. Caring babies: concern for others in distress during infancy. Dev Sci. 24, e13016 (2021).
Eisenberg, N. Empathy-Related Responding and Prosocial Behaviour. in Empathy and Fairness. (2008).
Zugasti, I. et al. CAR-T cell therapy for cancer: current challenges and future directions. Signal Transduct. Target. Ther. 10, 210 (2025).
Zehtabcheh, S. et al. Insights into KMT2A…