- Drinking Water Source May Influence Parkinson’s Disease Risk SciTechDaily
- Newer Groundwater Associated with Higher Risk of Parkinson’s Disease | Newswise Newswise
- Where you get your drinking water from can raise your risk of Parkinson’s by…
Category: 6. Health
-
Drinking Water Source May Influence Parkinson’s Disease Risk – SciTechDaily
-
“Canary in the Coal Mine:” Navigating the 2026 Measles Resurgence After Eliminating the Disease – Drug Topics
- “Canary in the Coal Mine:” Navigating the 2026 Measles Resurgence After Eliminating the Disease Drug Topics
- Measles outbreaks are costing the U.S. millions of dollars. The true losses can’t be counted. NBC News
- Measles cases surge in US, 12…
Continue Reading
-
European Guidance Advances Cardiovascular Risk Assessment – Medscape
- European Guidance Advances Cardiovascular Risk Assessment Medscape
- American College of Cardiology: Management of dyslipidemia in people living with HIV: The REPRIEVE paradigm in the 2025 ESC/EAS guidelines focused update European AIDS Treatment…
Continue Reading
-

5 Foods to Avoid if You Have Osteoporosis
What you eat and drink matters when you have osteoporosis. Diet accounts for about 25 percent of your risk for bone loss and fractures, according to Amy Joy Lanou, the director of the North Carolina Institute for Public Health and…
Continue Reading
-
Why Antifungal Drug Development Remains So Challenging According to John Rex, MD
Antimicrobial resistance is often discussed through the lens of bacteria, yet fungal pathogens present a distinct and increasingly urgent challenge. According to John Rex, MD, chief medical officer at F2G Ltd, in his interview with Infection…
Continue Reading
-

Schizophrenia Biomarkers Found in Cheek Swabs
A one-minute cheek swab could soon replace months of diagnostic uncertainty for millions of patients.
Researchers at Rutgers University have identified two key proteins in cheek cells that correlate with schizophrenia symptoms. This…
Continue Reading
-
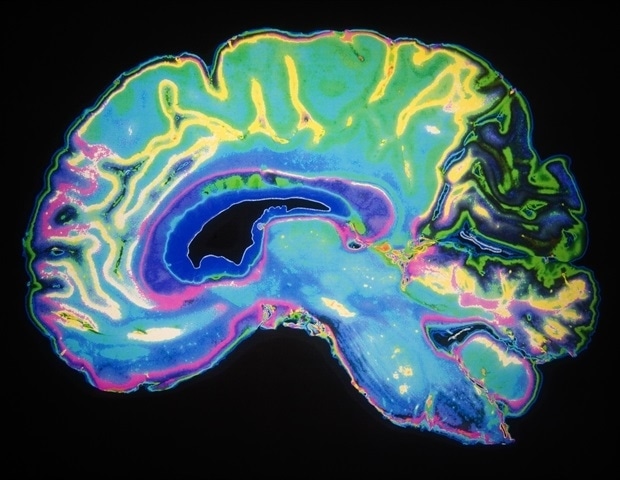
MSU scientists map the neural circuitry of drug compulsion
When a cocaine addict relapses, it isn’t a matter of personal failure – it’s the biological result of their brain’s rewiring, new research finds.
Michigan State University scientists found that cocaine changes how the hippocampus…
Continue Reading
-
Plain language summary of the management of certain side effects of teclistamab in people with multiple myeloma
This Plain language summary of publication article, published in Future Oncology, provides a breakdown of the strategies used in the MajesTEC-1 study to manage side effects that may occur with teclistamab treatment.
Access the full…
Continue Reading
-
Early Study of Lithium in Mild Cognitive Impairment Yields Mixed Outcomes – NeurologyLive
- Early Study of Lithium in Mild Cognitive Impairment Yields Mixed Outcomes NeurologyLive
- Trial Evaluates Lithium Treatment in Mild Cognitive Impairment European Medical Journal
- Lithium Might Slow Brain Decline Among Seniors, Pilot Study Shows
Continue Reading
