Introduction
Coronary atherosclerotic heart disease, also known as coronary heart disease (CHD), refers to heart conditions caused by the narrowing or obstruction of the coronary arteries due to atherosclerosis, leading to myocardial ischemia or…

Coronary atherosclerotic heart disease, also known as coronary heart disease (CHD), refers to heart conditions caused by the narrowing or obstruction of the coronary arteries due to atherosclerosis, leading to myocardial ischemia or…

“How did you sleep?” You might answer that question by weighing how many hours you slept or how often you woke up throughout the night.
But there is a third, often neglected, element of sleep to consider, experts say. It’s the consistency of…
A new scientific study has raised concerns over the long-term safety of the popular keto diet, which emphasizes high fat and very low carbohydrate intake to promote rapid weight loss.
Researchers warn that…
Duke researchers study approach that may help millions managing diabetic neuropathy and chemotherapy-induced nerve pain
For millions living with nerve pain, even a light touch can feel unbearable. Scientists have long suspected that…

Series B Co-led by New Investors Amplitude Ventures and ICG
MTX-474 Global Phase 2a study Initiated in Systemic Sclerosis (SSc)
MTX-463 Global Phase 2a Study in Idiopathic…

Biological systems like the heart typically display complex dynamical behaviour through interactions among components such as genes, proteins, or cells (Dana et al., 2008). These systems exhibit non-linear dynamics, feedback loops, and…
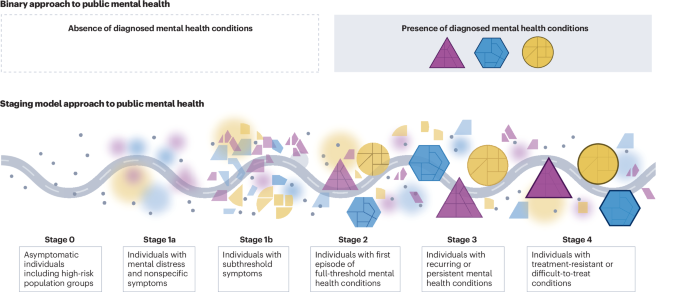
Herrman, H. et al. Time for united action on depression: a Lancet–World Psychiatric Association Commission. Lancet 399, 957–1022 (2022). This is an essential multidisciplinary contribution that underscores whole-of-society and…
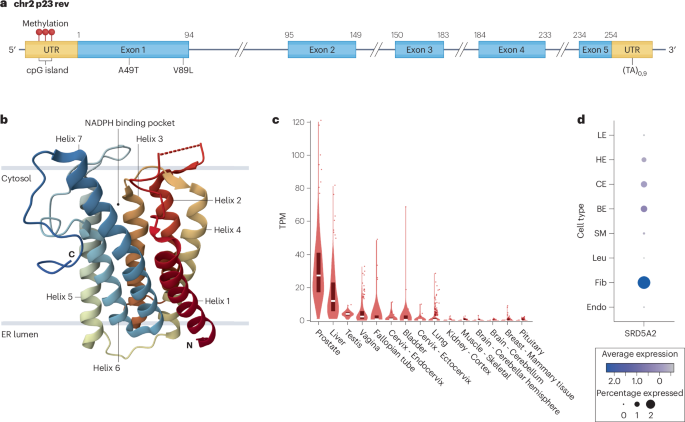
Brennen, W. N. & Isaacs, J. T. Mesenchymal stem cells and the embryonic reawakening theory of BPH. Nat. Rev. Urol. 15, 703–715 (2018).
Google Scholar
…

When an ant pupa has a deadly, incurable infection, it sends out a signal that tells worker ants to unpack it from its…

The bombshell announcement that the Trump administration no longer fully recommends a third of childhood vaccines means the US moved from leading globally on vaccination to lagging behind other high-income nations in preventing disease, experts…