- Pumpkin seeds support heart health, blood sugar balance, better sleep and hormone function.
- They’re rich in magnesium, zinc, protein, fiber and healthy fats—all in a small serving.
- Enjoy them in oatmeal, salads, smoothies or baked goods—or…
Category: 6. Health
-
What Happens to Your Body When You Eat Pumpkin Seeds
-
Common acne drug may protect against schizophrenia
A widely used antibiotic may help lower the chances of some young people developing schizophrenia, according to new research.
Scientists found that adolescents receiving mental health care who were prescribed the antibiotic doxycycline were…
Continue Reading
-
Just a moment…
Just a moment… This request seems a bit unusual, so we need to confirm that you’re human. Please press and hold the button until it turns completely green. Thank you for your cooperation!
Continue Reading
-
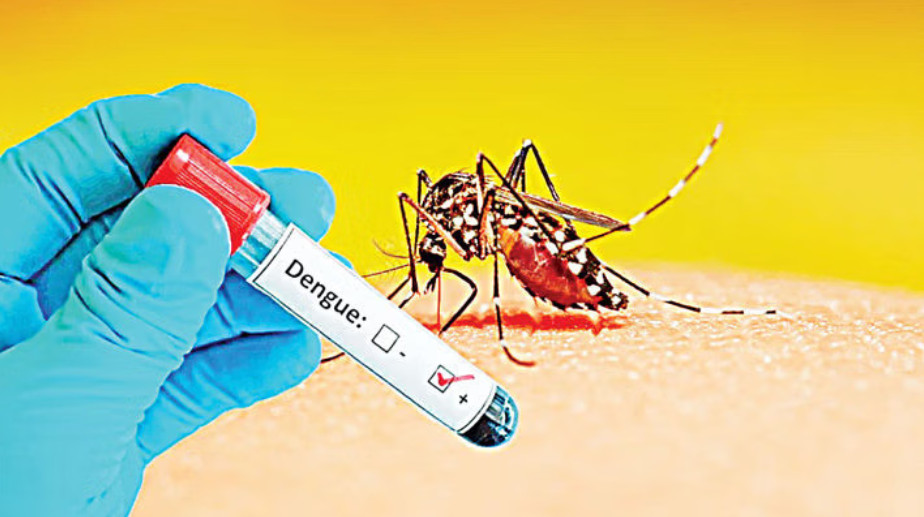
Why Bangladesh’s Chattogram sees a spike in dengue every November
DHAKA – Dengue cases have been rising sharply in Chattogram every November over the past few years, even though the disease usually peaks between July and October.
According to data from the Chattogram Civil Surgeon’s Office, 130 new cases…
Continue Reading
-

Perimenopause at 38? I felt robbed, says Emma Barnett
 Dan Kennedy
Dan KennedyBroadcaster Emma Barnett has said finding out she was going through perimenopause at the age of 38 felt like she had been “mugged, robbed”.
Barnett, now 40, said it was the “first time in my life I haven’t really wanted to be a woman -…
Continue Reading
-

Using Tobacco With Cannabis Is Tied to Unique Brain Changes, Small Study Finds : ScienceAlert
A preliminary investigation has found that those who use tobacco with cannabis show unique changes to their brain chemistry.
The findings could explain why those who use both often have worse addictions and mental health outcomes than those…
Continue Reading
-
Scientists unveil first draft of developing brain’s atlas – Dawn
- Scientists unveil first draft of developing brain’s atlas Dawn
- epDevAtlas: mapping GABAergic cells and microglia in the early postnatal mouse brain Nature
- New detailed brain growth atlas in mice offers insights into brain development Penn…
Continue Reading
-

Cambridge ‘swimming cap’ brings hope for brain-injured babies
Janine MachinEast of England technology correspondent, in Cambridge
 BBC
BBCResearchers say their “swimming cap”, which uses light and ultrasound to improve brain monitoring in newborns, is the first of its kind in the world Three-week-old Theo is fast…
Continue Reading
-

Higher levels of greenness associated with fewer hospital admissions for mental illness
Higher levels of greenness are associated with lower risks of hospital admissions for mental disorders, finds an analysis of data from seven countries over two decades, published in the BMJ’s climate issue today.
Local greenness…
Continue Reading
